Pedro Borghesi PoltronieriI; Andrea Cristina Oliveira FreitasII; Caroline Hamati Rosa BatistaI; Jorge Luiz Ribeiro da LuzII; Mayara Baschiera BarbosaII; Ricardo Siqueira GonçalvesII; Maria Carolina Martins SmanioI; Adilson Casemiro PiresIV
DOI: 10.21470/1678-9741-2022-0305
ABSTRACT
Introduction: Postoperative bleeding is one of the main causes of complications in cardiovascular surgery, which highlights the importance of ensuring adequate intraoperative hemostasis, providing a better patient outcome. This study aimed to improve the prevention of postoperative bleeding in the Cardiovascular Surgery Department of the Hospital Estadual Mário Covas (Santo André, Brazil) using an adapted version of the Papworth Haemostasis Checklist to assess the impact of this standardization on bleeding rate, postoperative complications, reoperation, and mortality.ACT = Activated clotting time
AFRVR = Atrial fibrillation with rapid ventricular response
AKI = Acute kidney injury
AMI = Acute myocardial infarction
BMI = Body mass index
CABG = Coronary artery bypass grafting
COVID-19 = Coronavirus disease 2019
CPB = Cardiopulmonary bypass
EuroSCORE = European System for Cardiac Operative Risk Evaluation
FBC = Full blood count
Hb = Haemoglobin
LA = Left atrium
LIMA = Left internal mammary artery
LV = Left ventricular
PA = Pulmonary artery
RA = Right atrium
RSPV = Right superior pulmonary vein vent
SVG = Saphenous vein graft
TEG = Thromboelastogram
INTRODUCTION
Checklists have gained importance in healthcare, being currently widely used in the surgical field to standardize complex processes and reduce the risk of errors. Thus, the use of a checklist in hemostasis procedures is presented as a simple, quick, and easy-to-use tool to prevent complications, yielding a better clinical outcome for patients[1,2].
Postoperative bleeding is one of the main potentially modifiable complications in cardiovascular surgeries[3] since both anemia and the need for transfusions of blood products can significantly increase patients’ mortality and morbidity[4-7]. Several studies show that blood transfusion can be harmful by increasing the chance of postoperative infection, myocardial and cerebrovascular ischemia, kidney injury, worse recovery, and death[8,9].
To reduce these modifiable factors, researchers in the United Kingdom developed a multidisciplinary intraoperative checklist, known as the Papworth Haemostasis Checklist. Its assessment is based on two major sections: operative sites and coagulation status. When comparing variables before and after the implementation of this checklist, there was a significant reduction in mediastinal blood loss, rate of return to operating room for hemostasis, and use of blood products. As a secondary outcome, a significant reduction in hospital costs was observed[1]. Thus, the benefit of the intervention proposed by the British researchers reinforces the need to standardize criteria related to risk of bleeding in patients undergoing cardiac surgery.
Nowadays, there are not similar checklists aiming to mitigate postoperative bleeding in Brazil, which leads to a mortality rate of 5.6%, that exceeds the global rate of 3%[10]. Therefore, the standardization of haemostasis procedures in the form of an easy-to-use tool, as the mentioned checklist, seems to be an adequate way to decrease the bleeding rate of cardiovascular surgery in our country. In this scenario, this study has the objective to improve the prevention of postoperative bleeding in the Cardiovascular Surgery Department of the Hospital Estadual Mário Covas (Santo André, Brazil) with the use of the hemostasis checklist proposed by the Royal Papworth Hospital, in a Brazilian adapted version, to assess the impact of this standardization in bleeding rate (24-hour drain output), postoperative complications, reoperation for bleeding, and mortality.
METHODS
A non-randomized clinical trial was developed at the Centro de Cirurgia Cardiovascular of the Hospital Estadual Mário Covas in a two-year interval. A non-probabilistic sample was obtained with all patients who underwent cardiac surgery (coronary artery bypass grafting, valve replacement, aortic dissection repair, and ventricular aneurysm repair) within the study period, regardless of sex, age, body mass index (BMI), European System for Cardiac Operative Risk Evaluation (EuroSCORE) II, ejection fraction, heart rate, comorbidities, or surgery priority (elective, urgent, or emergency). Patients who underwent heart transplantation or pulmonary thromboendarterectomy were excluded from the study.
Patients were divided into two groups: Group 1 (G1), patients operated without the use of the checklist, and Group 2 (G2), patients in which the hemostasis checklist proposed by the Royal Papworth Hospital was used (Figure 1). G1 patients were enrolled between November 2019 to June 2020. The checklist phase (G2) lasted from November 2020 to June 2021.
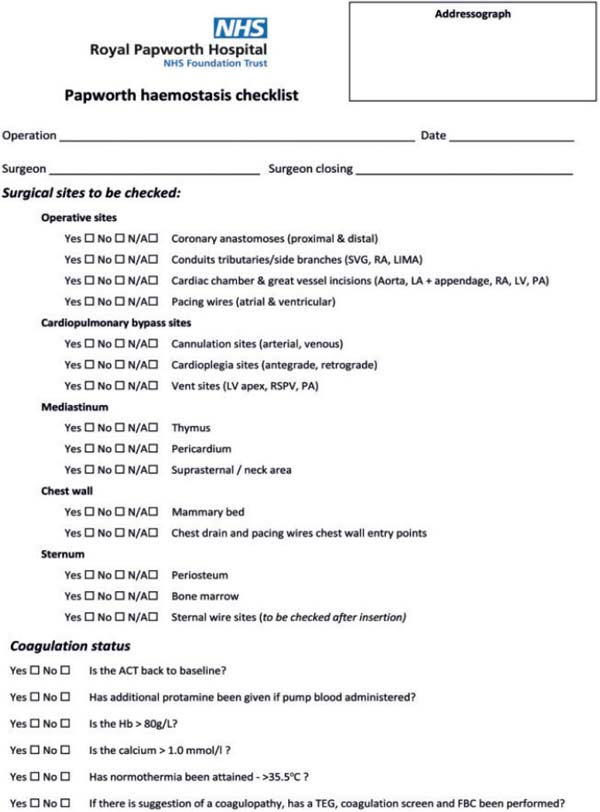
The Papworth Haemostasis Checklist was translated into Portuguese and adapted according to the measurement units (g/dL and mg/dL) used in Brazil and at the Hospital Estadual Mário Covas (Figure 2). This adapted version presents the same questions as the original checklist, except for the last question about the use of thromboelastography, which was not available at the hospital. The checklist was used intraoperatively, before the chest wall closure.
The adapted and translated version of the checklist was applied on a two-week period in order to access the feasibility of this new process in our service and to build an awareness culture on the new checklist as a tool to mitigate bleeding complications in our hospital. After this period, the surgical team had a debriefing to optimize the application of this checklist in the intraoperative routine. The major objective of this step was to evaluate how the team would deal with haemostasis revision using a standardized procedure. It was decided to not analyze the patients’ data in this step.
Preoperative data were collected in a standardized way and included demographic information (such as weight, height, and BMI), comorbidities (hypertension, diabetes mellitus, dyslipidemia, and smoking), left ventricular function, and EuroSCORE. In the postoperative evaluation, the chest tube drainage amount (mL) in the first 24 hours, the need for blood transfusions and reoperation for bleeding, intensive care unit and hospital length of stay, postoperative infection, and other complications were observed, as well as postoperative death. Patients were followed up for 30 days after surgery.
All patients were included in the study after written informed consent was obtained. The project was submitted and approved by the Research Ethics Committee of Centro Universitário FMABC (CAAE: 7122920.7.0000.0082).
A descriptive analysis of the data was performed, and, for qualitative variables, the absolute and relative frequencies were calculated. As the variables did not follow a normal distribution by the Shapiro-Wilk test, data were presented as mean and median.
To compare drainage output, amount of blood products, and days of hospitalization between groups, the Mann-Whitney U test was used. In relation to postoperative infection, death, and reoperation, Fisher’s exact test was used. A P≤0.05 was considered statistically significant. The analysis was performed using Stata software version 14.0.
RESULTS
A total of 200 patients were included in the study - 100 patients operated without the use of the checklist (G1) and 100 patients operated with this intervention (G2). Preoperative characteristics of both groups are described in Table 1.
| Group 1 | Group 2 | ||
|---|---|---|---|
| (N=100) | (N=100) | ||
| Gender | Female | 27 | 35 |
| Male | 73 | 65 | |
| Age (years) | Mean | 62.59 | 62.23 |
| Median | 63 | 63 | |
| BMI (kg/m2) | Mean | 27.34 | 27.19 |
| Median | 27.02 | 26.47 | |
| Surgery priority | Elective | 45 | 46 |
| Urgent | 48 | 53 | |
| Emergency | 7 | 1 | |
| Comorbidities | Hypertension | 83 | 83 |
| Diabetes | 42 | 46 | |
| Dyslipidemia | 19 | 17 | |
| No comorbidities | 16 | 14 | |
| Smoking | Non-smoker | 34 | 25 |
| History of smoking | 66 | 75 | |
| Heart rate | Normal sinus rhythm | 91 | 94 |
| Atrial fibrillation | 4 | 3 | |
| Other | 5 | 3 | |
| Ejection fraction | Preserved | 65 | 63 |
| Mid-range | 22 | 27 | |
| Reduced | 13 | 10 | |
| EuroSCORE II | Low risk (0-2 points) | 26 | 17 |
| Moderate risk (3-5 points) | 48 | 45 | |
| High risk (6-45 points) | 26 | 38 | |
BMI=body mass index; EuroSCORE=European System for Cardiac Operative Risk Evaluation
Regarding sex distribution in this study, there were a predominance of males and a higher mortality in male patients. Intraoperative characteristics of both groups are described in Table 2.
| Group 1 | Group 2 | ||
|---|---|---|---|
| (N=100) | (N=100) | ||
| Surgery performed | CABG | 86 | 94 |
| CABG + other surgery | 5 | 0 | |
| CABG + valve replacement | 5 | 2 | |
| Valve replacement | 2 | 2 | |
| Aneurysm/aortic dissection | 2 | 2 | |
| Cardiopulmonary bypass (CPB) | CPB use | 96 | 93 |
| CPB time (mean/median - min) | 65.80/33.17 | 70.58/31.40 | |
| Aortic cross-clamping time (mean/median - min) | 52.70/28.93 | 52.99/25.16 | |
CABG=coronary artery bypass grafting; CPB=Cardiopulmonary bypass
The checklist group (G2) had a shorter hospital stay and a lower bleeding volume, both without statistical significance. However, there was a greater need for blood transfusion. Table 3 shows postoperative state and clinical outcomes.
| Group 1 | Group 2 | P-value | |
|---|---|---|---|
| (N=100) | (N=100) | ||
| Chest tube drainage amount (mL) | 0.094 | ||
| Median (range) | 150 (0-1320) | 120 (0-2900) | |
| Mean | 214.67 | 189.5 | |
| Blood products transfusion | 0.765 | ||
| Transfused patients | 21 | 23 | |
| Packed red blood cells (mean) | 0.28 | 0.40 | |
| Platelets (mean) | 0.51 | 0.15 | |
| Cryoprecipitate (mean) | 0.33 | 0.07 | |
| Fresh frozen plasma (mean) | 0.22 | 0.02 | |
| Hospitalization (days) | 0.132 | ||
| Mean (minimum-maximum) | 10.64 (1-70) | 7.91 (1-40) | |
| Postoperative infection | 19 | 19 | 0.571 |
| Complications | 62 | 56 | 0.388 |
| Reoperation | 2 | 1 | 0.571 |
| Death | 8 | 2 | 0.050 |
Regarding postoperative infection in G1, nine patients had Coronavirus disease 2019 (COVID-19), eight had surgical site infection, eight had pneumonia, and two had urinary tract infection. There were single cases of pulmonary sepsis, sepsis of unknown origin, bloodstream infection, catheter-related infection, pseudomembranous colitis, and Clostridium difficile-associated diarrhea. In G2, eight patients had surgical site infection, four had pneumonia, two had urinary tract infection, and two had COVID-19. There were single cases of pulmonary sepsis, bloodstream infection, catheter-related infection, and colitis in G2.
Figure 3 shows the distribution of frequencies of non-infectious complications, of which five stand out.
Within the group of tachyarrhythmias and heart blocks, atrial fibrillation with rapid ventricular response (AFRVR) was the most prevalent, with 15 cases in G1 and 12 in G2.
There was a higher occurrence of reoperation in G1; in one patient, it was due to dehiscence of the aortic cannulation suture for cardiopulmonary bypass (CPB), and in another patient, it was due to cardiac tamponade after bleeding in the right atrium. In G2, the reoperated patient presented bleeding from aorta-saphenous vein anastomosis.
There were eight deaths in G1 and two deaths in G2. Of the eight deaths in G1, two occurred in patients who required reoperation.
DISCUSSION
There are several studies proposing surgical checklists, considering the benefits of this systematic methodology in reducing complications. However, few studies are focused on cardiac surgery, especially addressing the review of hemostasis processes. Considering this, in our study we chose to use a checklist aimed at this surgical time as proposed by the Royal Papworth Hospital. As in the British study, a reduction in mediastinal bleeding and reoperation for bleeding rates after use of the checklist was observed in the sample of our study, although the transfusion rate did not show a decrease[1].
By standardizing the steps of the final review of hemostasis, an individual failure of any item that goes unnoticed is prevented, which reduced the bleeding volume observed in this sample. However, a lower transfusion rate would be expected in the checklist group, something that was not observed in our study.
Comparing the two groups, the blood products transfusion rate practically remained the same, which may have occurred not only due to the patients’ preoperative state, with a high prevalence of chronic anemia, but also due to absence of a specific protocol such as the one discussed in the study by Bilecen et al[11]. These researchers adopted a specific transfusion protocol for cardiovascular surgeries that considered preand post-CPB red blood cell indices, adjusting the level of intervention according to the values found. This protocol reduced the transfusion of packed red blood cells and fresh frozen plasma, with better outcomes. Thus, that it would be interesting to add a hemostasis checklist to a blood transfusion protocol to obtain even more benefits.
Another advantage of the checklist use was the reduction of some complications directly related to a lower postoperative bleeding rate, of which the most significant is acute kidney injury (AKI), the second most common in our study, as shown in Figure 3. Brown et al.[12], in a retrospective study published in 2010, found a direct relationship between increased mortality and development of AKI in the postoperative period of cardiac surgery, and this rate was proportional to the duration of kidney injury. In our study, G2 patients had a lower incidence of AKI and mortality, in agreement with the work of Brown et al[12].
Tachyarrhythmias were frequent complications in our study and followed the same trend found in the literature. Conti et al.[13] showed that supraventricular tachyarrhythmias, especially AFRVR, can occur in 10 to 40% of patients after cardiac surgery, and their incidence is slightly higher in valve repair procedures. As seen in our study, the checklist did not have a significant impact on its reduction, since these conditions are related to the physiologic stress caused by myocardial manipulation during the procedure.
Although not directly related to bleeding rates, a lower incidence of pneumothorax was observed in G2 patients. The application of the checklist during chest wall closure implies a more detailed review of hemostasis and, during this review, a pneumothorax caused by pleural manipulation during the intraoperative period may have been diagnosed and treated early, avoiding the need for future pleural drainage in the intensive care environment, which would lead to longer hospital stay (which occurred with G1 patients).
Some studies showed results similar to ours regarding the reoperation for bleeding rate. Loor et al.[14] observed a significant reduction from 3.1 to 1.9% with the use of a checklist that assessed only sites of bleeding. Regarding reoperation, our service had a 2% rate before the checklist was implemented - within the world range (2-8%) and below the Brazilian average (3.7%). With the checklist, this rate presented values below the world average, reaching 1%[10,14].
Most studies carried out in the last two years have been affected by the COVID-19 pandemic. Surgeries performed during the activity of severe acute respiratory syndrome coronavirus 2 infection resulted in a worsening of surgical complications, especially pulmonary complications, and it was also likely to be associated with hemorrhagic complications. Wang et al.[15] demonstrated an increase in postoperative bleeding, need for blood transfusion, and mediastinal drainage after cardiovascular surgery in patients with COVID-19 when compared to healthy patients. In our study, the institutional protocol postponed surgery in all those who present a COVID-19 positive test preoperatively, so all infected patients acquired the disease in the postoperative period.
In our study, the use of the checklist was accompanied by a statistically significant reduction in deaths. The inclusion of other aspects to be checked regarding the perioperative performance of patients can enhance this result, as described by Spanjersberg et al[16]. By proposing a checklist with a broader view and assessment of risk factors, the authors obtained a significant mortality reduction in 120 days.
Stressing the importance of intraoperative bleeding control, in their study, Mazzeffi et al.[17] showed that 19.5% of deaths occurred due to complications from reoperations for bleeding. Corroborating this data and analyzing the impact of transfusion in these patients, Vivacqua et al.[18,19] suggested that transfusion and reoperation provided higher mortality and increased the risk of negative postoperative outcomes.
Limitations
This study has some limitations. We observed that adherence to the checklist seems to be a challenge. Thus, to achieve all these benefits, team training is essential. Part of the study period took place during the COVID-19 pandemic, which, in addition to delaying data collection and limiting the sample size, made it necessary to exclude deaths of patients diagnosed with COVID-19 in the postoperative period, whose complications could lead to biased results. The absence of thromboelastography in the checklist may have suppressed relevant intraoperative data and possibly affected the blood transfusion rate. The individual decision on indication of blood transfusion in cases of borderline red blood cell indices in this research may have been different from what occurred in the British research that inspired our study. A larger sample, through a multicenter study in Brazil, as well as randomization of the study can improve statistical relevance in the items assessed and refine the analysis of other variables.
CONCLUSION
The use of Papworth Haemostasis Checklist, adapted and translated into Portuguese, at the Centro de Cirurgia Cardiovascular of Hospital Estadual Mário Covas proved to be a simple and quick intervention to improve the prevention of postoperative bleeding, with an impact on number of deaths in the study period. The reduction in deaths was possible thanks to reduction in bleeding rate, postoperative complications, and reoperations for bleeding. In view of this, our service recommends implementation of similar hemostasis checklists in other centers. A multicenter, randomized study could improve statistical relevance of the items assessed as well as refine the analysis of other relevant variables.
REFERENCES
1. Ali JM, Gerrard C, Clayton J, Moorjani N. Reduced re-exploration andblood product transfusion after the introduction of the papworth haemostasischecklist†. Eur J Cardiothorac Surg. 2019;55(4):729-36.doi:10.1093/ejcts/ezy362. [MedLine]
2. Hales BM, Pronovost PJ. The checklist--a tool for error managementand performance improvement. J Crit Care. 2006;21(3):231-5.doi:10.1016/j.jcrc.2006.06.002. [MedLine]
3. van Boxtel AGM, van Veghel D, Soliman Hamad MA, Schulz DN, StepaniakPS, van Straten AHM. Use of an intraoperative checklist to decrease theincidence of re-exploration for postoperative bleeding after cardiac surgery.Interact Cardiovasc Thorac Surg. 2017;25(4):555-8.doi:10.1093/icvts/ivx130. [MedLine]
4. Rawn JD. Blood transfusion in cardiac surgery: a silent epidemicrevisited. Circulation. 2007;116(22):2523-4.doi:10.1161/CIRCULATIONAHA.107.739094. [MedLine]
5. Koch CG, Khandwala F, Li L, Estafanous FG, Loop FD, Blackstone EH.Persistent effect of red cell transfusion on health-related quality of lifeafter cardiac surgery. Ann Thorac Surg. 2006;82(1):13-20.doi:10.1016/j.athoracsur.2005.07.075. [MedLine]
6. Kuduvalli M, Oo AY, Newall N, Grayson AD, Jackson M, Desmond MJ, etal. Effect of peri-operative red blood cell transfusion on 30-day and 1-yearmortality following coronary artery bypass surgery. Eur J Cardiothorac Surg.2005;27(4):592-8. doi:10.1016/j.ejcts.2005.01.030. [MedLine]
7. van Straten AH, Bekker MW, Soliman Hamad MA, van Zundert AA, MartensEJ, Schönberger JP, et al. Transfusion of red blood cells: the impact onshort-term and long-term survival after coronary artery bypass grafting, aten-year follow-up. Interact Cardiovasc Thorac Surg. 2010;10(1):37-42.doi:10.1510/icvts.2009.214551. [MedLine]
8. Scott BH. Blood transfusion in cardiac surgery: is it appropriate?Ann Card Anaesth. 2007;10(2):108-12.doi:10.4103/0971-9784.37935. [MedLine]
9. Karthik S, Grayson AD, McCarron EE, Pullan DM, Desmond MJ.Reexploration for bleeding after coronary artery bypass surgery: risk factors,outcomes, and the effect of time delay. Ann Thorac Surg. 2004;78(2):527-34;discussion 534. doi:10.1016/j.athoracsur.2004.02.088.
10. Miana LA, Atik FA, Moreira LF, Hueb AC, Jatene FB, Auler Junior JA,et al. Risk Factors for postoperative bleeding after adult cardiac surgery. BrazJ Cardiovasc Surg. 2004;19(3):280-6.doi:10.1590/S0102-76382004000300005.
11. Bilecen S, de Groot JA, Kalkman CJ, Spanjersberg AJ, Moons KG,Nierich AP. Effectiveness of a cardiac surgery-specific transfusion protocol.Transfusion. 2014;54(3):708-16. doi:10.1111/trf.12346. [MedLine]
12. Brown JR, Kramer RS, Coca SG, Parikh CR. Duration of acute kidneyinjury impacts long-term survival after cardiac surgery. Ann Thorac Surg.2010;90(4):1142-8. doi:10.1016/j.athoracsur.2010.04.039. [MedLine]
13. Conti VR, Ware DL. Cardiac arrhythmias in cardiothoracic surgery.Chest Surg Clin N Am. 2002;12(2):439-60, viii.doi:10.1016/s1052-3359(02)00006-6.
14. Loor G, Vivacqua A, Sabik JF 3rd, Li L, Hixson ED, Blackstone EH, etal. Process improvement in cardiac surgery: development and implementation of areoperation for bleeding checklist. J Thorac Cardiovasc Surg.2013;146(5):1028-32. doi:10.1016/j.jtcvs.2013.05.043. [MedLine]
15. Wang X, Gao H, Zhang Z, Deng C, Yan Y, Shi T. Effect of the COVID-19 pandemic on complications and mortality of patients with cardiac surgery. J Cardiothorac Surg. 2021;16(1):361. doi:10.1186/s13019- 021-01744-z.
16. Spanjersberg AJ, Ottervanger JP, Nierich AP, Speekenbrink RGH, Stooker W, Hoogendoorn M, et al. Implementation of a specific safety check is associated with lower postoperative mortality in cardiac surgery. J Thorac Cardiovasc Surg. 2020;159(5):1882-90.e2. doi:10.1016/j.jtcvs.2019.07.094.
17. Mazzeffi M, Zivot J, Buchman T, Halkos M. In-hospital mortality after cardiac surgery: patient characteristics, timing, and association with postoperative length of intensive care unit and hospital stay. Ann Thorac Surg. 2014;97(4):1220-5. doi:10.1016/j.athoracsur.2013.10.040.
18. Vivacqua A, Koch CG, Yousuf AM, Nowicki ER, Houghtaling PL, Blackstone EH, et al. Morbidity of bleeding after cardiac surgery: is it blood transfusion, reoperation for bleeding, or both? Ann Thorac Surg. 2011;91(6):1780-90. doi:10.1016/j.athoracsur.2011.03.105.
19. Hansen LS, Ryhammer PK, Hjørnet NE, Jakobsen CJ. The 30-day mortality is a poor quality indicator. J Cardiothorac Vasc Anesth. 2017;31:S8-S9. doi:10.1053/j.jvca.2017.02.069.
Authors’Roles & Responsibilities
PBP= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
ACOF= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
CHRB= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
JLRL= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
MBB= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
RSG= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
MCMS= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
ACP= Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
Article receive on Tuesday, August 9, 2022
Article accepted on Tuesday, December 27, 2022
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license