Lucas Regatieri BarbieriI,V; Marcelo Luiz Peixoto SobralI,II,V; Glaucio Mauren da Silva GerônimoI,V; Gilmar Geraldo dos SantosI,II,III,VI; Evandro SbaraíniI,V; Fabio Kirsner DorfmanI,V; Noedir Antônio Groppo StolfI,IV,VI
DOI: 10.5935/1678-9741.20130073
ABSTRACT
INTRODUCTION: Postoperative atrial fibrillation is the most common arrhythmia in cardiac surgery, its incidence range between 20% and 40%.
OBJECTIVE: Quantify the occurrence of stroke and acute renal insufficiency after myocardial revascularization surgery in patients who had atrial fibrillation postoperatively.
METHODS: Cohort longitudinal bidirectional study, performed at Portuguese Beneficent Hospital (SP), with medical chart survey of patients undergoing myocardial revascularization surgery between June 2009 to July 2010. From a total of 3010 patients were weaned 382 patients that presented atrial fibrillation preoperatively and/or associated surgeries. The study was conducted in accordance with national and international following resolutions: ICH Harmonized Tripartite Guidelines for Good Clinical Practice - 1996; CNS196/96 Resolution, and Declaration of Helsinki.
RESULTS: The 2628 patients included in this study were divided into two groups: Group I, who didn't show postoperative atrial fibrillation, with 2302 (87.6%) patients; and group II, with 326 (12.4%) who developed postoperative atrial fibrillation. The incidence of stroke in patients was 1.1% without postoperative atrial fibrillation vs. 4% with postoperative atrial fibrillation (P<0.001). Postoperative acute renal failure was observed in 12% of patients with postoperative atrial fibrillation and 2.4% in the group without postoperative atrial fibrillation (P<0.001), that is a relation 5 times greater.
CONCLUSION: In this study there was a high incidence of stroke and acute renal failure in patients with postoperative atrial fibrillation, with rates higher than those reported in the literature.
RESUMO
INTRODUÇÃO: A fibrilação atrial pós-operatória é a arritmia mais comum em cirurgia cardíaca; estima-se sua incidência entre 20% e 40%.
OBJETIVO: Avaliar a incidência de acidente vascular encefálico e insuficiência renal aguda nos pacientes que apresentaram fibrilação atrial no pós-operatório de cirurgia de revascularização miocárdica.
MÉTODOS: Estudo coorte longitudinal, bidirecional, realizado no Hospital da Beneficência Portuguesa (SP), com levantamento de prontuários de pacientes submetidos à cirurgia de revascularização miocárdica, de junho de 2009 a julho de 2010. De um total de 3010 pacientes foram retirados 382 pacientes, que apresentavam fibrilação atrial no pré-operatório e/ou cirurgias associadas). O estudo foi conduzido em conformidade com as seguintes resoluções nacionais e internacionais: ICH Harmonized Tripartite Guidelines for Good Clinical Practice - 1996; Resolução CNS196/96; e Declaração de Helsinque.
RESULTADOS: Os 2628 pacientes incluídos neste estudo foram divididos em dois grupos: grupo I, que não apresentou fibrilação atrial no pós-operatório, com 2302 (87,6%) pacientes; e grupo II, com 326 (12,4%) que evoluíram com fibrilação atrial no pós-operatório. A incidência de acidente vascular encefálico nos pacientes foi de 1,1% sem fibrilação atrial no pós-operatório vs. 4% com fibrilação atrial no pós-operatório (P<0,001). Insuficiência renal aguda pós-operatória ocorreu em 12% dos pacientes com fibrilação atrial no pós-operatório e 2,4% no grupo sem fibrilação atrial no pós-operatório (P<0,001), ou seja, uma relação 5 vezes maior.
CONCLUSÃO: Neste estudo verificou-se alta incidência de acidente vascular encefálico e insuficiência renal aguda nos pacientes com fibrilação atrial no pós-operatório, sendo as taxas maiores que as referidas na literatura.
CVA: Cerebrovascular accident
CPB: Cardiopulmonary Bypass
CVD: Cardiovascular Diseases
COPD: Chronic obstructive pulmonary disease
APE: Acute Pulmonary Edema
AF: Atrial fibrillation
POAF: Postoperative atrial fibrillation
CHF: Congestive heart failure
ARF: Acute renal failure
SPSS: Statistical Package for Social Sciences
ICU: Intensive care unit
INTRODUCTION
Life expectancy has increased in Western countries. According to the last census of the IBGE (2011), the elderly population in Brazil is also increasing across the country. This aging population have produced a greater number of hospitalizations, particularly those related to the presence of cardiovascular disease (CVD) [1,2]. Atrial fibrillation in the Postoperative (POAF) of cardiac surgery is the most common arrhythmia [3], it is a supraventricular tachyarrhythmia characterized by uncoordinated atrial activation with consequent deterioration of atrial function [4]. Its incidence is estimated at 20% to 40% and are believed to occur most frequently between the second and the fifth day after surgery [4-7]. Physiopathologically, it involves multiple factors such as pre-existing heart degenerative changes, dispersion of atrial refractoriness, changes in the speed of atrial conduction and atrial transmembrane potential so as to prolong hypokalemia Phase 3 depolarization, increasing automative and decreasing the conduction speed, oxidative stress, inflammation, atrial fibrosis, excessive production of catecholamines, changes in autonomic tone and expression of connexins. These changes result in increased dispersion of atrial refractoriness as well as the formation of a pro-arrhythmic substrate [8].
The length of stay of patients who develop POAF increases, on average, two to four days compared to those who remained in sinus rhythm, and this disease is the leading cause of post-discharge cardiac [9] surgery hospital readmission. Cerebrovascular accident (CVA), acute renal failure (ARF), hypotension, acute pulmonary edema (APE), increased length of stay in the intensive care unit (ICU) and estimated $ 10,000 in additional costs are directly associated with complications POAF [7,10]. Its occurrence is also associated with increased twice cardiovascular morbidity and mortality (4.7% versus 2.1% in the short term) [6-11].
The wide variation in the incidence of stroke and ARF in the postoperative period between studies, has a multifactorial profile including different diagnostic criteria, study design, inclusion and exclusion criteria, patient profiles and the centers involved in the sample making it difficult the comparison between studies.
The incidence of ARF in cardiac surgery ranges from 3.5 % to 31.0 % [12-14], and the need for dialysis was present in 0.3% to 15.0% of cases. The presence of acute renal failure in these patients increases the mortality rate of 0.4% to 4.4% to 1.3% to 22.3% and when there is need for dialysis such rates reach 25.0% at 88.9% [12-14], making it an independent risk factor for mortality. This study aims to assess the incidence of stroke and acute renal failure in patients with POAF of coronary artery bypass grafting.
METHODS
Longitudinal cohort bidirectional study. The sample consisted of 3010 subjects greater than 18 years who underwent coronary artery bypass grafting at Hospital da Beneficência Portuguesa de São Paulo in June 2009 to July 2010 period. Inclusion criteria were patients aged > 18 years who underwent coronary artery bypass grafting without other associated procedures. Exclusion criteria were: submission of the patient to any type of concomitant cardiac or non-cardiac surgery; patients with chronic atrial fibrillation and/or congenital cardiac surgery. From a total of 3010 patients, 382 patients were excluded: 60 (1.99%) patients with preoperative arrhythmia (chronic or paroxysmal atrial fibrillation, atrial flutter), and 322 (10.7%) patients because they had associated procedures to CABG (Table 1).
ARF was defined as creatinine level at or above 2.2 mg/dl and the clearance creatinine lower than 60ml plasma/min/1,73m2.
For statistical analysis, we used the statistical package SPSS (Statistical Package for Social Sciences) for Windows, version 16.0, and R: A Language and Environment for Statistical Computing. All tests were performed with consideration of bilateral hypotheses, we assumed a significance level of α=5%. Initially we used descriptive statistics to assess the absolute and relative frequency, mean, standard deviation, median and interquartile range of the variables, with graphical presentation.
When checking the equality of proportions between groups on the variables studied, the chi-square test or Fisher's exact test were used, depending on the variable analyzed be qualitative or quantitative. Comparison between quantitative variables was performed using the Student t test or nonparametric Mann-Whitney test (when comparing two groups) or ANOVA or the nonparametric Kruskal-Wallis test (when comparing three or more groups) [15].
The project was submitted, reviewed and approved by the Research Ethics Committee of RBAPB, under protocol number 760-11 accepted on November 4, 2011. It was performed in accordance with the following national and international resolutions: ICH Harmonized Tripartite Guidelines for Good Clinical Practice - 1996; CNS196/96 Resolution, and the Declaration of Helsinki.
RESULTS
Patients included in this study (2,628) were divided into two groups: group I, who had no POAF, with 2,302 (87.6%) patients, and group II, with 326 (12.4%) patients who developed POAF. After assessing the predictive factors, we compared their evolution. The mean age of patients was 61.9+9.5 years. Eighteen hundred and thirty-six (69.9%) patients were male.
Table 2 shows the descriptive values of variables: indication for surgery, and of intraoperative, according to the groups with and without POAF, the intraoperative variables and surgical indication. Among these, the indication for urgent/emergency surgery proved to be one predisposing factor to the onset of POAF, which was 2.4% in those who underwent urgent/emergency surgery (group I: 16 to 0.7%, group II: 8 to 2.4 %, P=0.006).
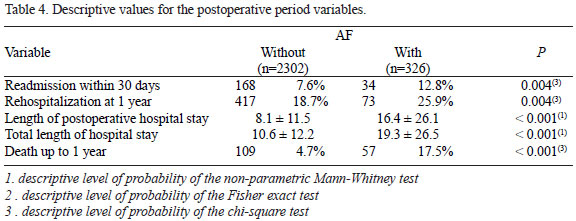
We found that the occurrence of cases with postoperative blood transfusion, stroke and ARF, rehospitalization at 30 days and at 1 year and death was significantly higher in patients with AF (Tables 3 and 4). In the group that evolved without the presence of AF the incidence of stroke and postoperative ARF was 1.1% and 2.4%, respectively, while this number was 4% and 12% in group II (with POAF) with P<0.001.
DISCUSSION
When we assessed the period in which the highest incidence of AF occurs, we found an average of 2.6 days with a median on day 2, which is in agreement with the literature [4-7]. As described by Leitch et al. [ 3], it was proved that age was a predisposing factor to a higher incidence of AF, with a P < 0.001. It was also proven its inference as a predisposing factor to increased incidence of POAF, and the average age in this group was six years older, showing a univariate assessment as an isolated predisposing factor to increased incidence of POAF. While in group I the mean age of patients was around 61 years old, in group II such average was around 67 years old.
Age is a risk factor widely cited and discussed in the literature [3,16,17], probably due to the higher content of collagen fibrillation in elderly patients and degeneration of the conduction system.
Relevant statistic data observed in this study was the appearance of almost double the cases of POAF in patients with CRF (4.7% versus 8.9%) and creatinine > 2.2 mg/dl (2.1% versus 4.9%), which indicates the close relationship of these as aggravating for the onset of POAF. The same proportion in those with chronic obstructive pulmonary disease (COPD) (6.2% versus 11%). Through study of preoperative prognostic factors we observed that age, male gender, COPD, congestive heart failure (CHF ) and creatinine > 2.2 mg/dl are risk factors for the occurrence of AF.
We found a significant association between POAF and higher incidence of stroke and postoperative ARF. Creswell et al. [ 11 ] reported that patients developing postoperative atrial fibrillation had a 3.3% incidence of stroke, while those who did not develop the incidence was only 1.4% (P<0.005). Our study revealed, in a statistically significant univariate analysis, a higher incidence in cases of patients who developed POAF (1.1% vs 4.0% group I group II, P<0.001).
Another aspect worth noting is that the incidence of ARF that is also higher in the group with POAF: 12%, versus only 4% in group I, or that is, an incidence three times higher. A study assessing risk factors for the occurrence of stroke, transient ischemic attack and ARF in the postoperative period of CABG surgery found that atrial fibrillation and low cardiac output were significantly related to those complications [10,11,18,19].
The presence of conditions that determine hypoperfusion and renal ischemia is directly related to the development of ARF and patients with reduced renal functional reserve, where there is a reduction in glomerular filtration rate without elevation of serum creatinine above normal values, and are more likely to develop AKI even with minor kidney injuries. Preoperative and intraoperative factors such as age, previous level of creatinine, diabetes mellitus, cardiac output, cardiopulmonary bypass time and the use of intra-aortic balloon influence the development of ARF [12-14,16].
The development of postoperative complications such as infection, bleeding, and use of nephrotoxic substances can cause the level of severity of AKI is higher. The manipulation of the aorta appears to be an important causal factor for stroke after cardiac surgery, either secondary to large emboli as well as a result of microemboli (shower embolism). It is likely that a better preoperative study of the aorta and a careful handling may help reduce this incidence, and this includes: improved diagnosis and treatment of aortic disease with epiaortic ultrasound or transesophageal echocardiography, care in the preparation of the proximal coronary anastomoses without aortic unclamping (minimizing the aortic trauma), and the use of "screens" for protection during aortic manipulation.
Moreover, a better understanding is needed with regard to the relative contribution of the CPB circuit to embolic events, especially arterial line filter. On the other hand, cerebral hypoperfusion, both intraoperative and during the immediate postoperative period should be avoided, especially in patients with prior stroke or cerebrovascular disease [18,20].
We observed that the occurrence of POAF is associated with a significantly increased length of hospital stay, according to the literature. The length of ICU stay was longer in the POAF group 16 days on average (P<0.001 ), 8 days higher when comparing the patients in group I (twice as long), confirming its impact on morbidity and mortality [10,11,17,18,21].
In the present study, the hospital mortality of patients with POAF was higher than expected mortality rate for this type of elective surgery. The readmission rate within 30 days, and readmission within 1 year had a high incidence in patients with atrial fibrillation. This observational finding is consistent with other studies which have attributed to AF increased risk for patients in both short- and long-term [9,11,19,21,22].
CONCLUSION
In this study there was a high incidence of stroke and acute renal failure in patients with POAF, with rates higher than those reported in the literature Once the groups are not fully comparable, a definitive conclusion would be observed after more detailed studies.
REFERENCES
1. Vegni R, Almeida GF, Braga F, Freitas M, Drumond LE, Penna G, et al. Complicações após cirurgia de revascularização miocárdica em pacientes idosos. Rev Bras Ter Intensiva. 2008;20(3):226-34.
2. IBGE - Instituto Brasileiro de Geografia e Estatística. Primeiros resultados definitivos do Censo 2010: população do Brasil é de 190.755.799 pessoas. Comunicação Social, 2011 [Acesso em: 02 set. 2011]. Disponível em:<http://www.ibge.gov.br/home/presidencia/noticias/noticia_visualiza.php?id_noticia=1866&id_pagina=1>
3. Leitch JW, Thomson D, Baird DK, Harris PJ. The importance of age as a predictor of atrial fibrillation and flutter after coronary bypass grafting. J Thorac Cardiovasc Surg. 1990;100(3):338-42. [MedLine]
4. Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; European Society of Cardiology Committee for Practice Guidelines; European Heart Rhythm Association; Heart Rhythm Society.. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(7):e257-e354. [MedLine]
5. Dunning J, Treasure T, Versteegh M, Nashef SA; EACTS Audit and Guidelines Committee. Guidelines on the prevention and management of de novo atrial fibrillation after cardiac and thoracic surgery. Eur Cardiothorac Surg. 2006;30(6):852-72.
6. Banach M, Misztal M, Goch A, Rysz J, Goch JH. Predictors of atrial fibrillation in patients following isolated surgical revascularization. A meta-analysis of 9 studies with 28786 patients. Arch Med Sci. 2007;3(3):229-39.
7. Filardo G, Hamilton C, Hebeler RF Jr, Hamman B, Grayburn P. New-onset postoperative atrial fibrillation after isolated coronary artery bypass graft surgery and long-term survival. Circ Cardiovasc Qual Outcomes. 2009;2(3):164-9. [MedLine]
8. Oliveira DC, Ferro CR, Oliveira JB, Prates GJ, Torres A, Egito ES, et al. Postoperative atrial fibrillation following coronary bypass graft: clinical factors associated with in-hospital death. Arq Bras Cardiol. 2007;89(1):16-21. [MedLine]
9. Lahey SJ, Campos CT, Jennings B, Pawlow P, Stokes T, Levitsky S. Hospital readmission after cardiac surgery. Does "fast-track" cardiac surgery result in cost saving or cost shifting? Circulation. 1998;98(19 Suppl):II35-40. [MedLine]
10. Chung MK, Asher CR, Dykstra D, Dimengo J, Weber M, Whitman G, et al. Atrial fibrillation increases length of stay and cost after cardiac surgery in low risk patients targeted for early discharge. J Am Coll Cardiol. 1996;27:9A.
11. Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993;56(3):539-49. [MedLine]
12. Mangos GJ, Brown MA, Chan WY, Horton D, Trew P, Whitworth JA. Acute renal failure following cardiac surgery: incidence, outcomes and risk factors. Aust N Z J Med. 1995;25(4):284-9. [MedLine]
13. Abel RM, Buckley MJ, Austen WG, Barnett GO, Beck CH Jr, Fischer JE. Etiology, incidence, and prognosis of renal failure following cardiac operations. Results of a prospective analysis of 500 consecutive patients. J Thorac Cardiovasc Surg. 1976;71(3):323-33. [MedLine]
14. Conlon PJ, Stafford-Smith M, White WD, Newman MF, King S, Winn MP, et al. Acute renal failure following cardiac surgery. Nephrol Dial Transplant. 1999;14(5):1158-62. [MedLine]
15. Rosner B. Fundamentals of biostatistics. Boston: PWS Publishers; 1986. 584p.
16. Amar D, Zhang H, Leung DH, Roistacher N, Kadish AH. Older age is the strongest predictor of postoperative atrial fibrillation. Anesthesiology. 2002;96(2):352-6. [MedLine]
17. Aranki SF, Shaw DP, Adams DH, Rizzo RJ, Couper GS, VanderVliet M, et al. Predictors of atrial fibrillation after coronary artery surgery: Current trends and impact on hospital resources. Circulation. 1996;94(3):390-7. [MedLine]
18. Engelman DT, Cohn LH, Rizzo RJ. Incidence and predictors of tias and strokes following coronary artery bypass grafting: report and collective review. Heart Surg Forum. 1999;2(3):242-5. [MedLine]
19. Narayan SM, Cain ME, Smith JM. Atrial fibrillation. Lancet. 1997;350(9082):943-50. [MedLine]
20. Mayr A, Knotzer H, Pajk W, Luckner G, Ritsch N, Dünser M, et al. Risk factors associated with new onset tachyarrhythmias after cardiac surgery: a retrospective analysis. Acta Anaesthesiol Scand. 2001;45(5):543-9. [MedLine]
21. Ommen SR, Odell JA, Stanton MS. Atrial arrhythmias after cardiothoracic surgery. N Eng J Med. 1997;336(20):1429-34.
22. Lima MAVB, Sobral MLP, Mendes Sobrinho C, Santos GG, Stolf NAG. Fibrilação atrial e flutter após operação de revascularização do miocárdio: fatores de risco e resultados. Rev Bras Cir Cardiovasc. 2001;16(3):244-50. View article
There was no financial support.
Authors' roles & responsibilities
LRB: Idealizer of the study
MLPS: Article Review
GMSG: Aid in medical records survey
GGS: Article Review
ES: Aid in medical records survey
FKO: Aid in the statistical part of the article
NAGS: Article Review
Article receive on Thursday, May 16, 2013
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license