Nei Antônio Rey0; Luiz Felipe Pinho Moreira0; David T Cheung0; Ivan Sérgio Joviano Casagrande0; Luiz Alberto BENVENUTI0; Noedir Antonio Groppo Stolf0
DOI: 10.1590/S0102-76382011000200020
ABSTRACT
OBJECTIVE: In an effort to make available homografts
preserved in a simpler and less costly way, we evaluated the
polyethyleneglycol, L-Hydro (LH) method, that consists in the controlled
extraction of antigenic substances and the incorporation of anti-inflammatory
and anti-thrombotic agent.
METHODS: We substituted the pulmonary trunk in ten ovines, seven
received LH treated pulmonary homografts and three, fresh pulmonary homografts,
orthotopically implanted and followed-up for 320 days. Ovines where evaluated
by means of laboratory tests, echocardiographic exams. At the 320 days, were
euthanized, hemodynamic, radiology, macroscopic, optic/electronic microscopic,
scanning/transmission evaluations were performed. Results were analyzed by
Student t test of independent samples for continuous data, by variance analysis
of repeated measures, and by Fisher exact test for categorical data.
RESULTS: We couldn't establish relevant differences in clinical
evolution and laboratory tests between groups. Echocardiogram revealed
difference in pulmonary medium gradient, which was significant 10 months
follow-up, higher in the control group. Radiologic and macroscopic evaluations
didn't established differences. In the optic/electronic microscopic evaluation,
liner and interstitial cells were equally found in both groups. The cell liner
percent calculated in both groups was similar. Cellularity nodules were
observed only infresh homograft group.
CONCLUSIONS: These data indicate that both groups presented similar
clinical/hemodynamic performances. The LH group's echocardiogram presented a
better performance. It also presented histological evidences of interstitial
and endothelial cell repopulation. In the macro/optic and electronic
microscopic analysis, group L-H presented macroscopy/histological structure and
ultra-structural similar to the fresh group, with the exception of nodules with
higher interstitial cellularity, present only in the fresh homograft group.
RESUMO
OBJETIVO:
Buscando novas formas de preservação de tecidos utilizamos o
polietileno-glicol, método L-Hydro (LH), que consiste na extração controlada de
substâncias antigênicas e incorporação de agente antinflamatório e
antitrombótico.
MÉTODOS: Em dez carneiros jovens, substituímos o tronco pulmonar, em
sete, por homoenxertos pulmonares (HP) tratados pelo processo L-H e, em três,
por HP a fresco, implantados ortotopicamente, seguidos por 320 dias. Os
carneiros foram avaliados por exames laboratoriais e ecocardiográficos. Ao cabo
dos 320 dias foram sacrificados, procedendo-se à avaliação hemodinâmica,
radiológica, macro/microscópica, óptica e eletrônica, varredura e transmissão.
Resultados foram analisados pelo teste t de Student de amostras independentes
para dados contínuos, análise de variância para medidas repetidas, pelo teste
exato de Fisher para dados categóricos.
RESULTADOS: Evolução clínica e exames laboratoriais não conseguiram
estabelecer diferenças significativas entre os grupos. Ecocardiograma revelou
diferença quanto ao gradiente médio pulmonar, significativa aos 10 meses, maior
no grupo controle. Avaliação radiológica e macroscópica não estabeleceu
diferenças. Na avaliação microscópica, óptica/eletrônica, células de
revestimento e intersticiais foram encontradas nos dois grupos igualmente. O
porcentual de revestimento celular calculado nos dois grupos foi semelhante.
Nódulos de celularidade foram observados somente no grupo de homoenxertos a
fresco.
CONCLUSÕES: Estes dados indicam que os dois grupos apresentaram
desempenho clínico e hemodinâmico semelhante. Ao ecocardiograma o grupo LH
apresentou melhor desempenho, e evidências histológicas de repopulação celular
intersticial e endotelial. Na análise macro/microscópica, óptica/eletrônica, o
grupo L-Hydro apresentou macroscopia, estrutura histológica e ultraestrutural
semelhante ao homoenxerto fresco, à exceção de nódulos de maior celularidade
intersticial, presentes apenas no homoenxerto a fresco.
INTRODUCTION
Several congenital or acquired heart diseases determine the need for heart valve replacement or valved conduit interposition. It is estimated that at least 60,000 valve replacements in the USA and 170,000 worldwide are performed each year [1]. The valve replacement changes the progress of the disease, bringing a new perspective to the patient. It is necessary to have a reliable valve substitute in order to accomplish this. For this reason, for over forty years surgeons have been trying to seek an ideal valve replacement. The first prostheses were mechanical. Right afterwards the aortic valve removed aseptically from a corpse was employed either using the lyophilization process as a preservation medium [2] or the Hanks solution [3]. The homografts were the ones, which showed good results in the short term. The breakthrough was the concept of the "bioprosthesis" [4], which associated biological material assembled on a metal or plastic base. The complications inherent to mechanical prostheses and bioprosthesis, such as thromboembolism and degeneration led to the return of the use of homografts. Nonetheless, the difficulty to obtain the homografts remained.
The current method of choice was the cryopreservation [5] with the homograft banks, a way to facilitate the availability and conservation. Even thus, some problems remain, such as the cost, sophistication of the method, the difficulty of eliminating infectious agents [6], and the degeneration in the long term [1,7,8]. Other processes, such as decellularization are under development with contradictory outcomes. The desire to provide homografts preserved in a simple and economical way, while maintaining the quality led us to evaluate a new form of preservation, with the use of polyethylene glycol (PEG), which has been used in the treatment of tissue from former times [9]. Therefore, we compared the pulmonary homograft morphologically and functionally treated by PEG, the L-Hydro method, with the fresh pulmonary homograft orthotopically implanted in sheep.
METHODS
Fourteen Santa Inês sheep (Ovis Aries) between 4 and 6 months of age and weighing between 18 and 32 kg of body weight were selected. The animals underwent general clinical examination by a veterinarian, and they considered clinically healthy for surgery intervention. In the preparation of the homografts, we used sheep obtained from a slaughterhouse approved by the Ministry of Agriculture and the Federal Inspection Service.
In the case of the L-Hydro homografts, all processing took place over a period of up to 36 hours of the death of the donor and consisted of the following phases:
1st phase - extraction of sheep antigens and masking of sheep antigens remaining under controlled chemical oxidation, by using polyethylene glycol acid;
2nd phase - incorporation to the graft of nonsteroidal anti-inflammatory drugs (equivalent to aspirin) and an antithrombotic agent (equivalent to heparin);
3rd phase - sterilization of tissue in aqueous hydrogen peroxide solution (H2O2).
Once the preservation process was completed, the grafts were stored in a 50% ethanol solution until its application. In fresh grafts, the hearts were obtained in an adjacent operating room, under sterile conditions. The pulmonary trunk was dissected from its bifurcation to its origin, preserving a small flap of muscular tissue from the right ventricle. The grafts were placed in a cold saline solution at 4ºC and immediately used for characterizing the grafts as "homovital grafts."
A left thoracotomy was performed in the fourth intercostal space (ICS). The animals were under general anesthesia and monitoring. Cardiopulmonary bypass (CPB) support was established at the RA-Ao under normothermia. The pulmonary trunk was resected. The valve was destroyed, and the homograft was interposed through a continuous suture with 4-0 monofilament thread. CPB was discontinued. The hemostasis was reviewed, and the drain was placed into the left hemithorax. The drain was removed after the closure of the chest, and pulmonary re-expansions were completed.
In the postoperative period, the animals received routine care and antibiotics. After 7 days in satisfactory clinical condition, they were transferred to the biotherium where they remained on daily basis observation by the veterinarian.
Laboratory tests (blood count, platelets, calcium, phosphorus, LDH) were performed, at 6 and 11 months and echocardiography at 7 and 10 months, assessing the mean and maximum pulmonary gradients, valve mobility and sufficiency. At 320 days an elective sacrifice was carried out under general anesthesia. At that time, the hemodynamic assessment was undertaken using a Swan-Ganz catheter. Central venous pressure (CVP), pulmonary artery pressure (PAP), pulmonary capillary wedge pressure (PCWP), cardiac output, and pulmonary arteriography were also analyzed. Then, through a new left thoracotomy, the piece was removed, proceeding to the macroscopic evaluation by three observers. The items analyzed [10] were: stenosis; insufficiency; dehiscence; presence of vegetation; ruptures/tear/ abrasion; thrombi on the cusps; thrombi in the aortic sinuses (sinuses of Valsalva); calcification in cusps; calcification in the aortic sinus (sinus of Valsalva); flexibility and thickening and coaptation of the cusps. Mammography was used to assess calcification. The pieces were radiographed all together. Then, the pieces were sent to be examined under light microscopy and scanning and transmission electron microscopy.
All the experiments were performed at the Research Center of Labcor Laboratories, with the approval of the Scientific Committee of the Heart Institute and Ethics Committee of the University of São Paulo Faculty of Medicine Clinics Hospital (a teaching hospital) and followed the norms of the Brazilian College of Animal Experimentation (Colégio Brasileiro de Experimentação Animal - COBEA). We adopted the Veterinary Anatomical Nomina.
Statistical analysis was performed using the software SPSS version 12.0. Continuous data are presented as mean and standard deviation and categorical data as scores. We avoided the use of percentages due to the small size of study groups. The statistical significance of differences was obtained by the independent samples Student's t test. Continuous data were analyzed using ANOVA and the Fisher exact test for categorical data. The level of significance was P <0.05.
RESULTS
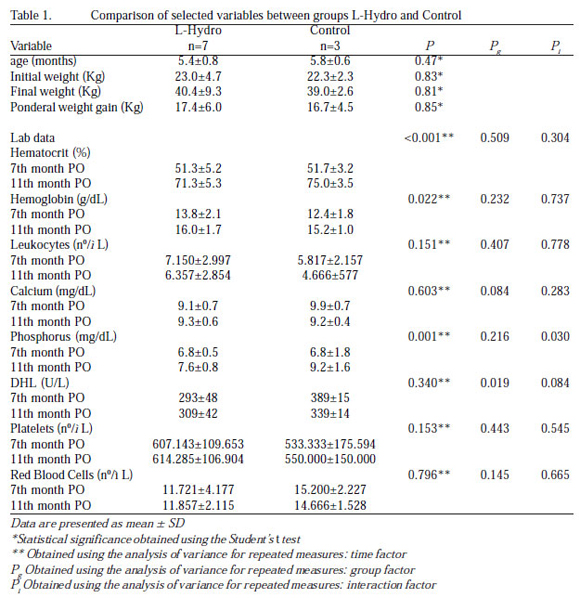
The homograft treated by the L-Hydro method has good flexibility, and it is easy to perform the suture interposition and presents good homeostasis. Of the 14 operated animals, 3 died within 24 hours. One animal suffered an accident on the postoperative day 7 and was sacrificed. The sample consisted of two groups: Group L-Hydro with seven animals, and the control group with three animals. One of the sheep from the L-Hydro group had an infection with the emergence of lumps in the neck. Treated with antibiotics, the animal improved and remained under observation throughout the study length of time. The other animals remained uneventful. Table 1 shows the data of initial and final weight, ponderal weight gain, and laboratory tests performed in both groups at 7 and 12 months. There were no significant differences between both groups regarding the laboratory tests and ponderal weight gain. Means, standard errors, the descriptive level of Student's t test, and the analysis of variance of these variables are shown in the same table.
The echocardiogram performed in 7 and 10 months demonstrated preserved ventricular function in all cases. Except for case number 1 of the L-Hydro group, in which the pulmonary valves were well visualized opening without restrictions. Right ventricle pressures and the grafts' diameter did not differ. The maximum and mean pulmonary gradient showed differences in the seventh month of the study, with higher values in the control group. This difference was significant in the tenth month of the study, with the control group presenting higher gradients. The mean, standard errors, the descriptive level of Student's t test, and the analysis of variance of these variables are presented in Table 2.

The hemodynamic analysis revealed no differences between groups in CVP, PAP, PCWP, and cardiac output. Table 2 presents mean, standard errors, and the descriptive level of Student's t test of the hemodynamic variables. At angiography, both groups presented sufficient homografts with valves of normal mobility and without stenoses, except for case number 1, L-Hydro Group, in which we found significant insufficiency. Mammography showed no radiopaque images suggestive of calcifications (high density) in the pulmonary semilunar cusps in both groups, but revealed radiopaque images, which were suggestive of calcification in the regions corresponding to the suture lines in both groups.
At macroscopic evaluation, the case number 1 of L-Hydro Group presented fibrinous vegetation, partially calcified, located in the aortic sinuses (sinuses of Valsalva), with destruction of the cusps. All other cases of both groups showed no stenosis, insufficiency, rupture, or dehiscence/abrasion. Both groups have also presented flexible, coapted, and thin cusps. The presence of thrombus in the cusp was found in one case of group L-Hydro, measuring 2x4 mm in a cusp. We have not identified a thrombus in the cusp in neither case in the control group. Thrombi in the aortic sinuses (sinuses of Valsalva) were observed in four cases in group L-Hydro and in all cases of the control group. Pulmonary valve calcification was found only in the case 1 of the L-Hydro Group and in no other case of both groups. Annular calcification was not confirmed in any case. Macroscopy photos are shown in Figure 1. The macroscopic variables examined are presented in Table 3. They analyzed using the Fisher's exact test.


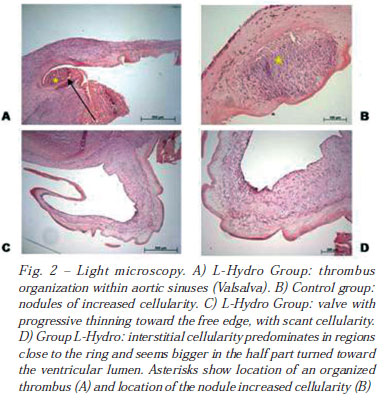
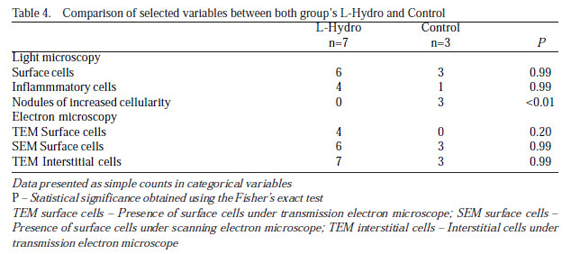
Light microscopy revealed rather retracted cusps with increasingly tapering toward the free edge, which generally presented scarce or absent cellularity and marked eosinophilic appearance. In general, the interstitial cellularity predominates in regions close to the ring and seems more exuberant in the middle part of the ring, which is turned to the ventricular lumen (spongy layer of the ventricle). However, nodules of greater interstitial cellularity were observed in intermediate areas of the cusps in three cases of the control group. Cells covering part of the surface of cusps were observed in all cases, except in the case number 1, on both surfaces (apparently predominating in the ventricular region), in both regions close to the ring and to the free edge. Parasitic cyst was detected in the myocardium of case number 1 (L-Hydro group): Sarcocystis spp, a common finding in sheep and not related to the infection presented by this animal. Light microscopy findings are shown in Figure 2.
The scanning electron microscopy showed in all cases but in case 1, surface areas paved by rounded or elongated cells, sometimes in a parallel arrangement, consistent with endothelial cells, presenting the appearance of normal endothelium of sheep found in the literature. Figure 3 shows the aspect found in our cases.

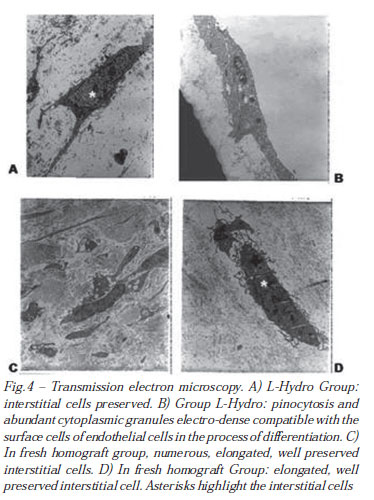
The transmission electron microscopy showed, in the midst of numerous collagen fibers, the presence of ultrastructurally intact, round, or elongated (most commonly) cells with many cytoplasmic projections. Nucleus with condensed chromatin was found in the periphery as well as a cytoplasm containing normal organelles. Electron-dense corpuscles could be seen in some of the organelles. Ultrastructural appearance consistent with viable mesenchymal cells, probably fibroblasts, could also be observed. In four cases of group L-Hydro, cells were observed partially coating the cusps.
Such cells were similar to those described earlier, presenting interdigitating cytoplasmic projections. In one these cases, it was observed the focal presence of the basement membrane below the mentioned cells, and cellular structures were present in two other cases. In one of these, noted the presence of abundant pinocytosis and electron-dense cytoplasmic granules in some of these surface cells. These features are consistent with endothelial cells, probably in the process of differentiation. The findings of transmission electron microscopy are illustrated in Figure 4. Table 4 summarizes the findings of light and electron microscopy. The Fisher's exact test was used to analyze the outcomes. In one of these, we observed the presence of abundant pinocytosis and electron-dense cytoplasmic granules in some of these surface cells. Such features are consistent with endothelial cells, probably in the process of differentiation. The findings of transmission electron microscopy are illustrated in Figure 4. Table 4 summarizes the findings of light and electron microscopy. The Fisher's exact test was used to analyze the outcomes.
DISCUSSION
The valve replacement or valved conduit interposition is an issue of great magnitude, due to the frequency in which they are required and their geographical distribution that is universal. It becomes necessary the use of valve artificial substitute of high quality because the success of the surgical procedure depends on it. Other important factors are availability and price of the artificial substitutes. By choosing the biological valve replacement, the ideal would be to use heterologous graft with some form of treatment because it is easily accessible, although the receptor immunological response anticipates being higher than for the use of homografts.
This attempt was performed using the Sinergraft method (Cryolife, Inc.), i.e., heterografts decellularized. After good experimental results, the clinical use has proven to be disastrous [11], thus being discontinued. The method keeps being employed in homografts with good results in the literature [12]. Decellularization of heterografts by the deoxycholic acid (DOA) shows good experimental [13] and clinical outcomes at a 24-month observation period [14]. A number of decellularization methods shows to be promising, such as the sodium dodecyl sulfate (SDS), which is used in homografts [15] as many other surface-active agents [16].
The outstanding method in clinical practice today, the cryopreservation, with proven results, although it is not the ideal, because it comes up against the complexity, high cost, difficulty of transport to remote regions, poor sterilization of some organisms, and degeneration in the long term, especially in young people [17,18]. So, anyway, the search continues. The L-Hydro method using polyethylene glycol (PEG), already tested in other types of tissue, presents itself as simple, inexpensive, and unsophisticated. The reduced toxicity of PEG was demonstrated by Wicomb et al. [19]. This substance was effective when added to the solution of myocardial preservation, ensuring the functional viability of the organ for a far greater length of time than that recommended for use with conventional cardioplegic solutions [20].
It is also attributed to PEG the immunosuppressive property, in which is based the L-Hydro preservation. Antigens that are combined with PEG manifest a reduction of antigenicity, as reported in the work of Collins et al. [21]. In Cheung's own words, "This is a process that turns the cells into non-viable cells, by not harming the extracellular structure and by not removing the cells, which differs from decellularization." In our study, we compared the L-Hydro group with a control group of "in fresh" homografts with the immediate use, real "homovital" grafts. We proceeded like this in order to have a reference comparison with the "gold standard" of the grafts, once the published clinical studies using "homovital" grafts show exceptional results, reaching up to 97% of the grafts free of degeneration in 10 years [22]. In the series of Yacoub, the clinical use of "homovital" homografts was an independent factor for reduced mortality [22]. It is known that any processing of grafts, including sterilization with low concentration of antibiotics has the potential to alter the viability as well as the physical and antigenic properties of the tissue [23]. We used juvenile sheep, in which the general cardiac structure is similar to human valves [24], once they are traditional research models [25], because they present early calcifications. One factor that has to be taken into account when analyzing the results is the low antigenic reaction of the sheep, for example. It is used blood among animals without testing the ABO/Rh, without any harmful consequence. We do not know how much of this fact may influence the repopulation found, once one of the clinically established mechanisms for the degeneration is undoubtedly the antigenic reaction [18]. The number of sheep complied with the International Standard Organization - ISO 5840, 3rd edition, published in 1996 and revised in 2005. We had three immediate deaths, and the sheep sacrificed at 7 days (due to an accident occurred, which dislocated the left front limb), was referred to postmortem examination, with the graft in good condition. Our echocardiographic results showed that the L-Hydro conservation was more favorable than the "in fresh/ homovital homograft," providing lower gradients in 10 months. Light microscopy showed "nodules of greater cellularity" only in fresh homografts, which is a finding found in the literature [26], and that we attributed to a recellularization via blood stream, that the L-Hydro method has not provided. Animal models, although with an anatomy very similar to the human anatomy, have different antigenicity, which can lead to results not reproducible when in the clinical practice.
CONCLUSION
The comparison of the pulmonary homograft conserved by the L-Hydro method with fresh homograft orthotopically implanted in juvenile sheep, followed-up during 320 days showed:
The homograft treated using polyethylene glycol (PEG) showed clinical and hemodynamic performance similar to fresh homograft. The echocardiographic performance was better;
The homograft treated using polyethylene glycol (PEG) showed histologic evidence of interstitial and endothelial cell repopulation;
The homograft treated using polyethylene glycol (PEG) showed an ultrastructural and histological structure similar to the fresh homograft, except for nodules of increased interstitial cellularity, which were present only in the fresh homograft.
REFERENCES
1. Schoen FJ, Levy RJ. Founder's Award, 25th Annual Meeting of the Society for Biomaterials, perspectives. Providence, RI, April 28-May 2, 1999. Tissue heart valves: current challenges and future research perspectives. J Biomed Mater Res. 1999;47(4):439-65. [MedLine]
2. Ross DN. Homograft replacement of the aortic valve. Lancet. 1962;2(7254):487. [MedLine]
3. Barrat-Boyes BG. Homograft aortic valve replacement in aortic incompetence and stenosis. Thorax. 1964;19:131-50. [MedLine]
4. Carpentier A. From valvular xenograft to valvular bioprosthesis: 1965-1970. Ann Thorac Surg. 1989;48(3 Suppl):S73-4. [MedLine]
5. O'Brien MF, Stafford G, Gardner M. The viable cryopreserved allograft aortic valve. J Card Surg. 1987;2(1 Suppl):153-67. [MedLine]
6. Peruzzo AM, Costa FDA, Abrahão WM. Controle microbiológico em valvas cardíacas humanas. Arq Bras Cardiol. 2006;87(6):778-82. [MedLine]
7. Koolbergen DR, Hazekamp MG, Heer E, Bruggemans EF, Huysmans HA, Dion RA, et al. The pathology of fresh and cryopreserved homograft heart valves: an analysis of forty explanted homograft valves. J Thorac Cardiovasc Surg. 2002;124(4):689-97. [MedLine]
8. Mitchell RN, Jonas RA, Schoen FJ. Pathology of explanted cryopreserved allograft heart valves: comparison with aortic valves from orthotopic heart transplants. J Thorac Cardiovasc Surg. 1998;115(1):118-27. [MedLine]
9. Wicomb WN, Hill JD, Avery J, Collins GM. Optimal cardioplegia and 24-hour heart storage with simplified UW solution containing polyethylene glycol. Transplantation. 1990;49(2):261-4. [MedLine]
10. Sayk F, Bos I, Schubert U, Wedel T, Sievers HH. Histopathologic findings in a novel decellularized pulmonary homograft: an autopsy study. Ann Thorac Surg. 2005;79(5):1755-8. [MedLine]
11. Simon P, Kasimir MT, Seebacher G, Weigel G, Ullrich R, Salzer-Muhar U, et al. Early failure of the tissue engineered porcine heart valve SYNERGRAFT in pediatric patients. Eur J Cardiothorac Surg. 2003;23(6):1002-6.
12. Tavakkol Z, Gelehrter S, Goldberg CS, Bove EL, Devaney EJ, Ohye RG. Superior durability of SynerGraft pulmonary allografts compared with standard cryopreserved allografts. Ann Thorac Surg. 2005;80(5):1610-4. [MedLine]
13. Dohmen PM, Costa F, Yoshi S, Lopes SV, Souza FP, Vilani R, et al. Histological evaluation of tissue-engineered heart valves implanted in the juvenile sheep model: is there a need for in-vitro seeding? J Heart Valve Dis. 2006;15(6):823-9. [MedLine]
14. Konertz W, Dohmen PM, Liu J, Beholz S, Dushe S, Posner S, et al. Hemodynamics characteristics of the Matrix P decellularized xenograft for pulmonary valve replacement during the Ross operation. J Heart Valve Dis. 2005;14(1):78-81. [MedLine]
15. Navarro FB, Costa FDA, Mulinari LA, Pimentel GK, Roderjan JG, Vieira ED, et al. Avaliação do comportamento biológico de homoenxertos valvares pulmonares descelularizados: estudo experimental em ovinos. Rev Bras Cir Cardiovasc. 2010;25(3):377-87. [MedLine] View article
16. Costa F, Dohmen P, Vieira E, Lopes SV, Colatusso C, Pereira EWL, et al. Operação de Ross com homoenxertos valvares decelularizados: resultados de médio prazo. Rev Bras Cir Cardiovasc. 2007;22(4):454-62. [MedLine] View article
17. Rajani B, Mee RB, Ratliff NB. Evidence for rejection of homograft cardiac valves in infants. J Thorac Cardiovasc Surg. 1998;115(1):111-7. [MedLine]
18. Lopes SAV, Costa FDA, Paula JB, Dhomen P, Phol F, Vilani R, et al. Análise do comportamento biológico de heteroenxertos descelularizados e homoenxertos criopreservados: estudo em ovinos. Rev Bras Cir Cardiovasc. 2009;24(1):15-22. [MedLine] View article
19. Wicomb WN, Perey R, Portnoy V, Collins GM. The role of reduced glutathione in heart preservation using a polyethylene glycol solution, Cardiosol. Transplantation. 1992;54(1):181-2. [MedLine]
20. Bhayana JN, Tan ZT, Bergsland J, Balu D, Singh JK, Hoover EL. Beneficial effects of fluosol-polyethylene glycol cardioplegia on cold, preserved rabbit heart. Ann Thorac Surg. 1997;63(2):459-64. [MedLine]
21. Collins GM, Wicomb WN, Levin BS, Verma S, Avery J, Hill JD. Heart preservation solution containing polyethyleneglycol: an immunosuppressive effect? Lancet. 1991;338(8771):890-1. [MedLine]
22. Yacoub M, Rasmi NR, Sundt TM, Lund O, Boyland E, Radley-Smith R, et al. Fourteen-year experience with homovital homografts for aortic valve replacement. J Thorac Cardiovasc Surg. 1995;110(1):186-93.
23. Lund O, Chandrasekaran V, Grocott-Mason R, Eiwidaa H, Mazhar R, Khaghani A, et al. Primary aortic valve replacement with allografts over twenty-five years: valve-related and procedure-related determinants of outcome. J Thorac Cardiovasc Surg. 1999;117(1):77-90. [MedLine]
24. Burman SO. Heterologous heart valves: past, present, and future. Ann Thorac Surg. 1989;48(3 Suppl):S75-6. [MedLine]
25. Gallegos RP, Nockel PJ, Rivard AL, Bianco RW. The current state of in-vivo pre-clinical animal models for heart valve evaluation. J Heart Valve Dis. 2005;14(3):423-32. [MedLine]
26. Hazekamp MG, Koolbergen DR, Braun J, Sugihara H, Cornelisse CJ, Goffin YA, et al. In situ hybridization: a new technique to determine the origin of fibroblasts in cryopreserved aortic homograft valve explants. J Thorac Cardiovasc Surg. 1995;110(1):248-57. [MedLine]
Article receive on Wednesday, January 26, 2011
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license