Monir ABBASZADEH
DOI: 10.1590/S0102-76382011000200017
ABSTRACT
OBJECTIVE: Although the overall complication rate has been
decreased significantly in recent years, stroke is a severe complication after
coronary bypass operations. The purpose of this study is to evaluate the
influence of carotid artery disease on the results of patients under CABG
operation.
METHODS: In a retrospective cohort study, 1,978 patients under CABG
operation were studied in Shariati Hospital between April 2002 and March 2006.
The patients who had only valve replacement or non-CABG procedure were excluded
from this study. As part of preoperative evaluation, carotid duplex
ultrasonography scans were performed. In order to estimate the degree of
carotid arteries stenosis, ultrasound imaging measurement and velocity criteria
were considered. The patients were classified into three groups: those with no
significant stenosis of the internal carotid artery (ICA) (moderate) group A,
those with significant stenosis (sever) group B and those with the occluded ICA
(critical) group C. Finally, all data were analyzed by SPSS software.
Statistical analyses were performed using the following testes; chi-square,
Fisher exact and Student's t tests.
RESULTS: The distribution of the 1,978 patients undergoing CABG
operation were as follows: group A = 1,938, group B = 30, and group C = 10. The
results of the evaluations show that perioperative stroke rates were 1.2% (24
patients) in group A, 0.4% (eight patients) in group B and 0.3% (six patients)
in group C (P<0.0001). Furthermore, perioperative mortality rates for
groups A, B and C were 0.1% (two patients), 0.3% (five patients) and 0.4%
(seven patients), respectively (P<0.0001).
CONCLUSION: The stroke and mortality in patients undergoing CABG are
increased when ICA occlusion is present.
RESUMO
OBJETIVO:
Embora a taxa de complicação geral tenha diminuído
significativamente em anos recentes, o acidente vascular cerebral é uma
complicação grave após operações de
revascularização do miocárdio. O objetivo deste estudo
é avaliar a influência da doença da artéria
carótida nos resultados de pacientes submetidos à
operação de revascularização do miocárdio
(CABG).
MÉTODO: Em um estudo de coorte retrospectivo, 1.978 pacientes
submetidos à revascularização do miocárdio foram
estudados no Shariati Hospital, entre abril de 2002 e março de 2006. Os
pacientes que tiveram apenas substituição da valva ou um
procedimento sem revascularização do miocárdio foram
excluídos do estudo. Como parte da avaliação
pré-operatória, foram realizados exames com ultrassonografia
Doppler dupla (dúplex) de artéria carótida. Na estimativa
do grau de estenose das artérias carótidas, foram considerados
critérios de mensuração de imagem de ultrassom e de
velocidade. Os pacientes foram classificados em três grupos: aqueles sem
estenose significativa (moderada) da artéria carótida interna,
grupo A; aqueles com estenose significativa (grave), grupo B; e aqueles com
oclusão (crítica) da artéria carótida interna,
grupo C. Finalmente, todos os dados foram analisados usando-se o programa SPSS.
Análises estatísticas foram realizadas usando-se os testes do
qui-quadrado, exato de Fisher e t de Student.
RESULTADOS: Dos 1.978 pacientes submetidos à
revascularização do miocárdio, 1.938 eram do grupo A, 30
do grupo B e 10 do grupo C. Os resultados das avaliações
mostraram que as taxas de acidente vascular cerebral perioperatórias
foram de 1,2% (24 pacientes) no grupo A, 0,4% (oito pacientes) no grupo B e
0,3% (seis pacientes) no grupo C (P < 0,0001). Além do mais,
as taxas de mortalidade perioperatórias para os grupos A, B e C foram
0,1% (dois pacientes), 0,3% (cinco pacientes) e 0,4% (sete pacientes),
respectivamente (P < 0,0001).
CONCLUSÃO: O acidente vascular cerebral e a mortalidade em
pacientes submetidos à revascularização do
miocárdio aumentam quando há oclusão da artéria
carótida interna.
INTRODUCTION
Carotid artery stenosis (CAS) is present in 10%-20% of patients undergoing coronary artery bypass grafting (CABG) and accounts for 30% of stroke associated with CABG [1], whereas the stroke event rate for asymptomatic patients with significant carotid artery stenosis ranges from 2%-5% [2-6]. Its etiology is multifactorial, including cerebral embolization from iatrogenic mobilization of atherosclerotic plaques, air/fat embolism, peripheral vascular disease (PVD), hemodynamic fluctuations, cerebral hyperthermia, aortic dissection, particular microemboli, emboli because of aortic arch disease, aortic "crunch" occurring with cross-clamping or cannulation, air and fat emboli [7-10] and systemic inflammatory reaction [11]. In spite of that, concomitant carotid artery disease may be very important in the etiology of perioperative stroke in patients undergoing CABG.
Previous studies greatly differ in their reports on perioperative stroke frequency for patients with internal carotid artery (ICA) occlusion or stenosis. Some of these reports have shown no increased risk of ipsilateral stroke in patients undergoing CABG [10,12,13]. On the other hand, some other reports have reported increased frequency (15%) of the perioperative transient ischemia (TIA) or cerebrovascular accident [3]. Due to these conflicting reports, it seems difficult to manage the patients with severe concomitant carotid stenosis/occlusion and coronary artery disease, and there are controversies regarding the methods of surgical treatment.
Carotid endarterectomy (CEA) in the presence of uncorrected coronary disease has been associated with very high operative mortality (20%) mainly due to myocardial infarction [14,15]. Similarly, coronary revascularization in the presence of severe carotid disease is associated with increased risk (14%) of perioperative stroke [5]. Originally, Bernhard et al. [14] proposed combined coronary revascularization and carotid endarterectomy in patients who had severe coronary and carotid artery disease, in order to reduce the morbidity and mortality in these patients. There have been a number of studies, which have addressed the question of synchronous management of patients having severe coronary artery disease and significant stenosis of ICA.
Some of these studies suggest that there was no significant increase in morbidity and mortality in patients undergoing simultaneous CEA and CABG [16,17]. Nevertheless, other studies have reported higher incidence of perioperative strokes when CEA and CABG procedures were combined than when they were operated in stages [18]. Current ACC/AHA guidelines recommend prophylactic carotid endarterectomy (CE) to reduce the risk of perioperative stroke in patients with CAS, who are scheduled for CABG.
This recommendation is based mainly on the results of several randomized studies of patients with general carotid artery stenosis, which compared CE with medical treatment for stroke prevention [1].
The purpose of this retrospective study was to evaluate the perioperative stroke rate and mortality among patients who underwent coronary bypass surgery and had internal carotid artery stenosis or occlusion.
METHODS
After the Institutional Review Board approval, the retrospective review was undertaken from April 2002 to March 2006, in which 1,978 patients undergoing CABG were investigated at our institution. Those patients who had only valve replacement or non-CABG procedure were excluded from this study. Carotid duplex ultrasonography scans were performed at an ICAVL accredited laboratory as part of preoperative evaluation of these patients. In order to estimate the degree of stenosis of the carotid arteries, ultrasound imaging measurement and velocity criteria were considered. A technologist estimated the degree of stenosis as percent of diameter reduction after collecting images in transverse and longitudinal sections and confirming image findings with peak systolic velocity and/or end diastolic velocity measurements. This method has been validated by comparison with independent magnetic resonance angiography (MRA) [19].
The results of the ultrasonography were available to all medical personnel and the written reports became part of a medical record. Depending on the results of preoperative carotid duplex ultrasonography study, these patients were divided into three groups: those with no significant stenosis of the ICA (moderate) group A; those with significant stenosis (severe) group B; and those with an occluded ICA (critical) group C.
Distribution of hypertension, diabetes, and smoking in each group is shown in Table 1. Perioperative stroke was defined as a persistent focal or multifocal neurologic deficit that was explained by ischemia of brain or brain stem, from the time of surgery until 30 days postoperatively and confirmed by computed tomography (CT) scan. All data were analyzed by SPSS software. Statistical analysis was conducted using either the chi-square test or Fisher exact test, when it was appropriate for categorical variables or the Student t tests for continuous variables. All P values were two-tailed. A P < 0.05 was considered statistically significant.

RESULTS
Of the 1,978 patients undergoing CABG, 1,938 (98%) patients had moderate ICA stenosis (group A), 30 (1.5%) had severe ICA stenosis (group B), and 10 (0.5%) had an occluded ICA (critical) group C. In the severe group, there were two patients who had contralateral ICA stenosis. In groups A and C, no patient had bilateral significant ICA stenosis. Distribution of hypertension, diabetes, and smoking in each group is shown in Table 1. The mortality rate among total patients was 0.7%. Table 1 shows the mortality and stroke rate in each group. The mortality rate among group C was 0.3% (P<0.0001). The pump time and cross-clamp time among various groups is shown in Table 2.

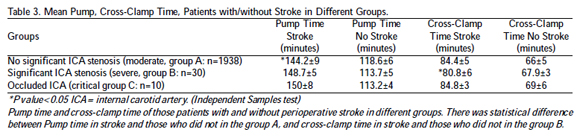
The mean pump time was higher in those patients who had a stroke as compared with those who did not have a stroke in the group A in Table 3 (P<0.05). Similarly, the cross-clamp time during coronary bypass was higher among patients who had a stroke as compared with those who did not have a stroke in group B (P<0.05). In Table 4, the pump perfusion pressure during the surgery in patients who had a stroke in the group A was less than the patients who did not have a stroke in a similar group (P<0.05).

DISCUSSION
Bernhard et al. [14], in 1972, reported the first series of patients having simultaneous CEA and CABG. In this study, they had suggested that the combined procedure decreases the mortality and morbidity. Hertzer et al. [20] in their prospective randomized trial divided CABG patients with carotid artery disease into three groups. One group of patients had preliminary CEA prior to CABG; in the second group, patients had simultaneous CABG/CEA; and in the third group, patients had delayed CEA after CABG.
In this study, the perioperative stroke in the first group was 4.2%, in the second group was 4.7% and in the last group was 7.4%. This study has suggested that delayed CEA was associated with higher perioperative strokes compared with patients who had preliminary CEA prior to CABG or simultaneous CEA and CABG. Other studies have shown an increase in perioperative stroke rate among patients who had either CEA or CABG as a staged procedure as compared with those who had CABG/CEA as a combined procedure.
Barnes [21] reviewed all patients with asymptomatic carotid artery disease and coronary artery revascularization submitted to stage procedures, in which a carotid endarterectomy was carried out as a first operation versus a synchronous operation. There were 1,483 patients in their study; the overall perioperative stroke was 2.9%. The perioperative stroke rate was 3.1% in stage carotid first and 2.8% in synchronous operations. A strategy of combined carotid endarterectomy and cardiac surgery had been adopted in the past. Staged carotid artery stenting prior to cardiac surgery is a less invasive alternative and seems to be associated with a lower incidence of stroke and myocardial infarction as compared to the combined surgical approach [22].
In our study, we found no difference in morbidity and mortality in patients having combined procedure (CABG+CEA) or CEA alone. All these patients had significant ICA stenosis (severe group B). However, these patients were not randomized. Prophylactic carotid endarterectomy can exclusively prevent 40% of strokes and only 7% of post-CABG strokes can be attributed to surgically correctable carotid disease [17]. Prophylactic carotid endarterectomy is still a matter of debate for asymptomatic patients, but it is a known fact that symptomatic and asymptomatic significant occlusive carotid disease is a major risk factor for perioperative stroke in patients who have undergone open-heart surgery. There is limited information available regarding the morbidity and mortality of patients with an occluded ICA having coronary bypass surgery.
In the recent report of Bucerius et al. [23] the overall incidence of stroke was 4.6% and varied between surgical procedures (CABG 3.8%, beating heart surgery CABG 1.9%). In a multicenter trial conducted by John et al. [24] incidence of stroke after open heart surgery was reported as 1.4%. Pompilio et al. [25] reported 4.8% stroke rate following CABG.
Similarly, Mickleborough et al. [26] in their prospective study showed the incidence of perioperative stroke among CABG patients who had unilateral ICA occlusion was 16.6% (2 of 12); whereas among patients with bilateral ICA occlusion, the perioperative stroke rate was 100% (1 of 1). In their study, they had shown that major neurological morbidity occurred in 14% of patients with unilateral occlusion of carotid artery, 20% of patients with significant carotid artery stenosis contralateral to an internal carotid artery occlusion, and 33% of patients with bilateral internal carotid occlusion. In a recent study, Tunio et al. [10] included 61 CABG patients having an occluded carotid artery; the incidence of perioperative stroke in these patients was 6.5% and the mortality rate was 8.6%.
In our study of 1978 CABG patients, there were 1938 in the group A, 30 in group B and 10 in the group C. The results of the evaluations show that perioperative stroke rates were 1.2% (24 patients) in the group A, 0.4% (eight patients) in group B and 0.3% (six patients) in group C (P<0.0001). Furthermore, perioperative mortality rates for groups A, B, and C were 0.1% (two patients), 0.3% (five patients) and 0.4% (seven patients), respectively (P<0.0001). This suggests that patients with ICA occlusion are indeed more prone to perioperative stroke and mortality. Recently, Schoof et al. [27] reported that typical strokes in ICA patients undergoing on-pump CABG were caused by decreased cerebral perfusion pressure and impaired cerebral autoregulation to compensate for the additional blood pressure decrease.
Mickleborough et al. [26] in their study included nine patients who had internal carotid occlusion and significant carotid artery stenosis on a contralateral side. All these patients had CABG and CEA; the perioperative stroke among these patients was 33% (3 of 9). Rizzo et al. [28] made a similar observation. They had 20 patients in their study who had significant carotid artery disease with contralateral occlusion of ICA; all these patients had CABG and CEA as a combined procedure. The perioperative stroke in this group was 15% (3 of 20).
Similarly, Tunio et al. [10] in their study had two patients in the occluded ICA group, which had CEA for significant ICA stenosis on a contralateral side. Both patients had a perioperative. These data suggest that CEA for contralateral significant carotid stenosis in the presence of ICA occlusion increases the risk of perioperative stroke. All perioperative strokes in the occluded ICA group were on the ipsilateral side as the occlusion. The mechanism of the strokes in these patients includes an embolism from the heart via collateral circulation such as the external carotid artery or from the blind stump of the occluded ICA. Low flow could be an important factor in these patients.
Henriksen et al. [29] measured the regional cerebral blood flow during CABG using the intra-arterial XE133. They found a decrease of 33% in cerebral blood flow during CABG. This decrease was attributed to hypothermia and hypocarbia. In a study conducted by D'Ancona et al. [11], as documented, the carotid artery disease and history of previous stroke can result in CVA through intraoperative or perioperative cerebral hypoperfusion. We have examined other variables, such as pump time, cross-clamp time, perfusion pressure and flow, during coronary bypass surgery among our three groups to find any association with perioperative stroke.
We found a significant difference among these groups (Table 2). Pump time, mean cross-clamp time and pump perfusion pressures during coronary bypass were higher in patients with significant carotid artery stenosis as compared with no significant carotid artery stenosis (P<0.0001). The mean pump time (Table 3) was higher in those patients who had a stroke (144 minutes) as compared with those who did not have a stroke (118 minutes) in the group A (P<0.05). Similarly, the cross-clamp time during coronary bypass was higher among patients who had a stroke (80 minutes) as compared with those who did not have a stroke (67 minutes) in group B (P<0.05). The pump perfusion pressure (Table 4) during the surgery was less among patients who had a stroke (63, 63mmHg) as compared with those who did not have a stroke (80, 82 mmHg) in groups A and B, respectively (P<0.05).
There was no significant difference in flow during coronary bypass in those who had a stroke (3110, 3074, and 3087 mL/min) as compared with those who did not have a stroke (3396, 3417, and 3360 mL/min) in groups A, B, and C, respectively (Table 4). Limitations of the present study include those inherent to retrospective, non-randomized data collection.
CONCLUSION
The presence of severe carotid stenosis and carotid artery occlusion increases the perioperative stroke and death rate among patients undergoing coronary artery bypass surgery. Both morbidity and mortality were higher in CABG patients who had occluded carotid artery (critical) as compared with those who had moderate carotid stenosis (<50%) and with those who had severe carotid stenosis. The knowledge of the risk factors offers an opportunity to implement preoperative and intraoperative measures as well as to reduce the occurrence of stroke, and it should influence the patient selection. We also suggest that more studies be conducted on synchronous CABG and CAE or a suitable method of surgery be found for these patients to reduce the mortality rate.
ACKNOWLEDGEMENT
We acknowledge the financial support received from Tehran University of Medical Sciences & Health Services Grant.
REFERENCES
1. Manabe S, Shimokawa T, Fukui T, Fumimoto KU, Ozawa N, Seki H, et al. Influence of carotid artery stenosis on stroke in patients undergoing off-pump coronary artery bypass grafting. Eur J Cardiothorac Surg. 2008;34(5):1005-8. [MedLine]
2. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid stenosis. JAMA. 1995;273(18):1421-8. [MedLine]
3. Hennerici M, Hülsbömer HB, Hefter H, Lammerts D, Rautenberg W. Natural history of asymptomatic extracranial arterial disease. Results of a long-term prospective study. Brain. 1987;110(Pt 3):777-91. [MedLine]
4. Ozatik MA, Göl MK, Fansa I, Uncu H, Küçüker SA, Küçükaksu S, et al. Risk factors for stroke following coronary artery bypass operations. J Card Surg. 2005;20(1):52-7. [MedLine]
5. O'Hollerhan LW, Kennelly MM, McClurken M, Johnson JM. Natural history of asymptomatic carotid plaque. Five year follow-up study. Am J Surg. 1987;154(6):659-62. [MedLine]
6. Norris JW, Zhu CZ, Bornstein NM, Chambers BR. Vascular risks of asymptomatic carotid stenosis. Stroke. 1991;22(12):1485-90. [MedLine]
7. Bounds JV, Sandok BA, Barnhorst DA. Fatal cerebral embolism following aorto-coronary bypass graft surgery. Stroke. 1979;7(6):611-4.
8. Branthwaite MA. Prevention of nerological damage during open-heart surgery. Thorax. 1975;30(3):258-61. [MedLine]
9. Chiarello L, Tomai F, Zeitani J, Versaci F. Simultaneous hybrid revascularization by carotid stenting and coronary artery bypass grafting. Ann Thorac Surg. 2006;81(5):1883-5. [MedLine]
10. Tunio AM, Hingorani A, Ascher E. The impact of an occluded internal carotid artery on the mortality and morbidity of patients undergoing coronary artery bypass grafting: a critical review of the literature. Eur J Vasc Endovasc Surg. 2002;23:283-94. [MedLine]
11. D'Ancona G, Saez de Ibarra JI, Baillot R, Mathieu P, Doyle D, Metras J, et al. Determinants of stroke after coronary artery bypass grafting. Eur J Cardiothorac Surg. 2003;24(4):552-6. [MedLine]
12. Barnes RW, Leibman PR, Marszalek PB, Kirk CL, Goldman MH. The natural history of asymptomatic carotid disease in patients undergoing cardiovascular surgery. Surgery. 1981;90(6):1075-83. [MedLine]
13. Breslau PJ, Fell G, Ivey TD, Bailey WW, Miller DW, Strandness DE Jr. Carotid arterial disease in patients undergoing coronary artery bypass operation. J Thorac Cardiovasc Surg. 1981;82(5):765-7. [MedLine]
14. Bernhard VM, Johnson WD, Peterson JJ. Carotid artery stenosis. Association with surgery for coronary artery disease. Arch Surg. 1972;105(6):837-40. [MedLine]
15. Ennix CL Jr, Lawrie GM, Morris GC Jr, Crawford ES, Howell JF, Reardon MJ, et al. Improved results of carotid endarterectomy in patients with symptomatic coronary disease: an analysis of 1,546 consecutive carotid operations. Stroke. 1979;10(2):122-5. [MedLine]
16. Darling RC 3rd, Dylewski M, Chang BB, Paty PS, Kreienberg PB, Lloyd WE, et al. Combind carotid endarterectomy and coronary artery bypass grafting does not increase the risk of preoperative stroke. Cardiovasc Surg. 1998;6(5):448-52. [MedLine]
17. Naylor AR, Mehta Z, Rothwell PM, Bell PR. Carotid artery disease and stroke during coronary artery bypass: a critical review of the literature. Eur J Vasc Endovasc Surg. 2002;23(4):283-94. [MedLine]
18. Kolh PH, Comte L, Tchana-Sato V, Honore C, Kerzmann A, Mauer M, et al. Concurrent coronary and carotid artery surgery: factors influencing perioperative outcome and long-term results. Eur Heart J. 2006;27(1):49-56. [MedLine]
19. Salles-Cunha S, Ascer E, Lorenson E. A carotid ultrasonography (US) and magnetic resonance angiography (MRA) comparison. J Ultrasound Med. 1996;15:S1-S117. [MedLine]
20. Hertzer NR, Loop FD, Beven EG, O'Hara PJ, Krajewski LP. Surgical staging for simultaneous coronary and carotid disease: a study including prospective randomization. J Vasc Surg. 1989;9(3):455-63. [MedLine]
21. Barnes RW. Asymptomatic carotid disease in patients undergoing major cardiovascular operations: can prophylactic endarterectomy be justified? Ann Thorac Surg. 1986;42(6 Suppl):S36-40. [MedLine]
22. Chan AW. Current perspectives on carotid revascularization among patients who need cardiac surgery. J Invasive Cardiol. 2010;22(8):386-90. [MedLine]
23. Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75(2):472-8. [MedLine]
24. John R, Choudhri AF, Weinberg AD, Ting W, Rose EA, Smith CR, et al. Multicenter review of preoperative risk factors for stroke after coronary artery bypass grafting. Ann Thorac Surg. 2000;69(1):30-5.
25. Pompilio G, Lotto AA, Agrifoglio M, Antona C, Alamanni F, Spirito R, et al. Nonembolic predictors of stroke risk in coronary artery bypass patients. World J Surg. 1999;23(7):657-63. [MedLine]
26. Mickleborough LL, Walker PM, Takagi Y, Ohashi M, Ivanov J, Tamariz M. Risk factors for stroke in patients undergoing coronary artery bypasses grafting. J Thorac Cardiovasc Surg. 1996;112(5):1250-8.
27. Schoof J, Lubahn W, Baeumer M, Kross R, Wallesch CW, Kozian A, et al. Impaired cerebral autoregulation distal to carotid stenosis/occlusion is associated with increased risk of stroke at cardiac surgery with cardiopulmonary bypass. J Thoracic Cardiovasc Surg. 2007;134(3):690-6.
28. Rizzo RJ, Whittemore AD, Couper GS, Donaldson MC, Aranki SF, Collins JJ Jr, et al. Combined carotid and coronary revascularization: the preferred approach to the severe vasculopath. Ann Thorac Surg. 1992;54(6):1099-108.
29. Henriksen L, Hjelms E, Lindeburgh T. Brain hyperperfusion during cardiac operations. Cerebral blood flow measured in man by intra-arterial injection of xenon 133: evidence suggestive of intraoperative microembolism. J Thorac Cardiovasc Surg. 1983;86(2):202-8. [MedLine]
Article receive on Monday, October 11, 2010
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license