INTRODUCTION
Development of aneurysmal thoracic collateral arteries has been rarely reported in the literature [1]. We aim to present a case of an adult patient with coarctation of the aorta with a previous distal aortic arch to descending aorta bypass that was referred for surgery due to residual coarctation and development of multiple aneurysmal subclavian to aortic collateral arteries.
CASE REPORT
A 47 year-old man with coarctation of the aorta underwent an aortic arch to descending aortic bypass with a 10-millimeter dacron graft through a left thoracotomy 10 years ago. He complained of atypical chest discomfort irradiated to the back, frequent palpitations and he was found to have uncontrolled hypertension on physical exam. Chest computed tomography [Figure 1] revealed a severely obstructed extra-anatomic bypass through a juxta ductal coarctation of the aorta, and multiple left subclavian artery to descending aorta aneurysmal collateral arteries (maximum diameter 45 millimeters).
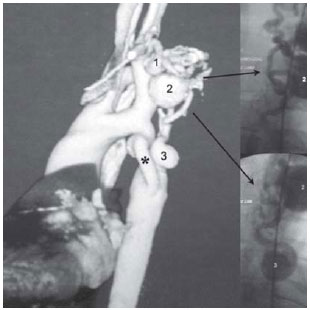
Fig. 1 - Preoperative chest computed tomography with three-dimensional reconstruction (left image), showing obstructed extra-anatomic bypass (*) and multiple aneurysmal thoracic collateral arteries (1,2,3) corresponding to their angiographic appearance on the right-sided images
Although the anatomic repair was initially contemplated as a primary option, the presence of a previous thoracotomy, with known aneurysmal collateral arteries and possibly dense adhesions changed our plan. Under general anesthesia, a median sternotomy was constructed, and a 26-millimeter ascending aorta to descending aortic knitted double velour graft (Boston Scientific, Natick, MA) was performed with the aid of standard cardiopulmonary bypass. His postoperative recovery was unremarkable, being discharged home on the eighth day in good condition.
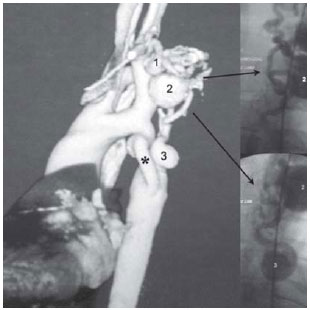
Control chest computed tomography six weeks later showed a patent graft and complete involution of all aneurysmal collateral arteries [Figure 2]. A year later, he is currently asymptomatic and in normotensive state.

Fig. 2 - Postoperative chest computed tomography with three-dimensional reconstruction, showing patent ascending aorta to descending aorta extra-anatomic bypass (§), the previous obstructed graft (*) and involution of all aneurysms
Development of collaterals in intercostals arteries and internal thoracic arteries is a common phenomenon in untreated coarctation of the aorta [2]. These arteries connect the subclavian artery or costocervical trunk to the descending aorta. There is a direct correlation with patient age at presentation, morphology of the coarctation and transverse arch and concomitant cardiac defects. However, the occurrence of aneurysmal collateral arteries in supra-aortic position is rare and it may have relation to the previous surgical approach. They probably represent hypertrophied preexisting normal vessels of an embryologic origin [3].
Indication for surgery in the present case was related to the risk of aneurysm expansion with extrinsic compression of adjacent structures, arterial rupture and pseudoaneurysm formation, in addition to deleterious effects of untreated coarctation.
There was a debate whether the anatomic repair in addition to collateral arteries ligation or embolization would provide better long-term outcomes. Although we generally favor the anatomic repair, this particular problem seemed to be better managed with an extra-anatomic bypass through a median sternotomy, avoiding manipulation of a densely adherent and well-vascularized area. Those factors are often responsible for extensive lung manipulation, airway injury and parenchyma hematomas. Aortic repair is usually demanding, which increases the risk of bleeding and paraplegia. Therefore, deep hypothermic circulatory arrest may be advocated [4]. In this setting, extra-anatomic bypass is a reasonable option in order to lessen surgical risk, eventually permitting simultaneous treatment of cardiac problems and to promote a sustained long-term distal aortic perfusion [5].
Percutaneous intervention is another treatment option and it has been particularly indicated in recurrent coarctation [6]. However, as opposed to children, adult patients often present with fragile, atherosclerotic and calcified aortas, which certainly limits procedure success and poses patients at additional risk.
Once the hemodynamic problem was fixed through an extra-anatomic bypass, there was complete involution of aneurysmal collateral arteries over the course of several weeks. Therefore, collateral arteries ligation or embolization does not appear to be justified.
REFERENCES
1. Lee AD, Shyamkumar NK, Nayak S, Agarwal S, Perakath B. Collateral artery aneurysm: a unique presentation of thoracic outlet syndrome. Eur J Vasc Endovasc Surg. 2005;29(6):611-2. [
MedLine]
2. Mathew R, Simon G, Joseph M. Collateral circulation in coarctation of aorta in infancy and childhood. Arch Dis Child. 1972;47(256):950-3. [
MedLine]
3. Kirks DR, Currarino G, Chen JT. Mediastinal collateral arteries: important vessels in coarctation of the aorta. AJR Am J Roentgenol. 1986;146(4):757-62. [
MedLine]
4. Lange R, Thielmann M, Schmidt KG, Bauernschmitt R, Jakob H, Hasper B, et al. Spinal cord protection using hypothermic cardiocirculatory arrest in extended repair of recoarctation and persistent hypoplastic aortic arch. Eur J Cardiothorac Surg. 1997;11(4):697-702. [
MedLine]
5. Oliveira SA, Lisboa LA, Dallan LA, Abreu Filho CA, Rochitte CE, Souza JM. Extraanatomic aortic bypass for repair of aortic arch coarctation via sternotomy: midterm clinical and magnetic resonance imaging results. Ann Thorac Surg. 2003;76(6):1962-6. [
MedLine]
6. Preventza O, Wheatley GH 3rd, Williams J, Hughes K, Ramaiah VG, Rodriguez-Lopez JA, et al. Endovascular approaches for complex forms of recurrent aortic coarctation. J Endovasc Ther. 2006;13(3):400-5. [
MedLine]

 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license