CLINICAL DATA
Full-term male baby at 2.49 kg from Limeira do Oeste, Minas Gerias, Brazil. Mother with 32 years of age who used carbamazepine. In the neonatal period, the baby was diagnosed with genetic disorder possibly due to constant hypercalcemia, congenital heart disease, right inguinal hernia and fimosis. The baby had follow-up visits with a cardiologist until 7 years and 9 months of age, at which point he was at 27 kg and when he started to present fatigue during moderate and great efforts. The patient was referred to surgery, and also presented difficulties with reading and writing from a mild cognitive defect; he was very kind, and had a small nose and full lips (due to his syndrome).
Physical examination revealed a good condition of the patient: eutrophic, afebrile, acyanotic. Regular cardiac rhythm, high murmur +++/6+ at left and right sternal margin, without opening snap and palpable fremitus in the sternal furcula. Normal pulmonary auscultation. Weak abdomen, liver at 1cm from the right costal edge, no palpable spleen, presence of normal hydro-aereal sounds without abdominal murmurs. Palpable and symmetric pulses in the extremities.
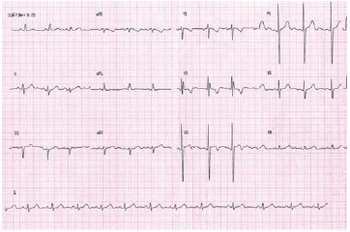
ELECTROCARDIOGRAM
Sinus arrhythmia, heart rate of 72bpm, SÂP +60º, SÂQRS -30°, PR 0.16s, QTC 0.42s. Left atrial overload, conduction disorder in the right branch evidenced at V2. RSR' pattern with QRS duration of 0.10s, in addition to an alteration of the anterior septal ventricular repolarization (Figure 1).
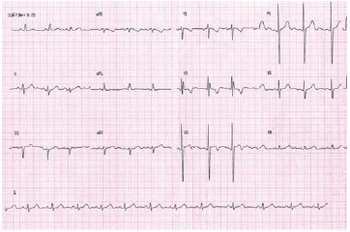
Fig. 1 - Electrocardiogram showing left ventricular overload due to supravalvar aortic stenosis
Visceral
situs solitus with levocardia. Normal heart area with cardiothoracic index of 0.51. Pulmonary vascular network unchanged.
ECHOCARDIOGRAM
Situs solitus with levocardia. The venoatrial, atrioventricular and ventriculo-arterial connections were all normal. Aortic ring measured 16mm, and the Valsalva sinus, 26mm; sinotubular stenotic region of 11mm, and 20mm ascending aorta. According to Doppler, the peak gradient was 80 mmHg with a mean of 44 mmHg. Supravalvar aortic stenosis with moderate left ventricular concentric hypertrophy.
DIAGNOSIS
The genetic confirmation of Williams-Beuren syndrome in the neonatal period led to the possibility of the evolution of supravalvar aortic stenosis, which occurs in approximately 75% of patients with heart disease, excluding patients with pulmonary artery stenosis, aorta coarctation and mitral valve regurgitation. Such involvement (which may be localized or diffused) is associated with chromosome 7, and more precisely with the elastin gene [1.2].
Rigorous clinical follow-ups were mandatory, because the best time for surgery had to be diagnosed during a clinical presentation: worsening of dyspnea - associated with the aggravation of the electrocardiographic and echocardiographic elements - left ventricular hypertrophy and increased risk of syncope and sudden death, in addition to guide to the better surgical technique to be used.
OPERATION
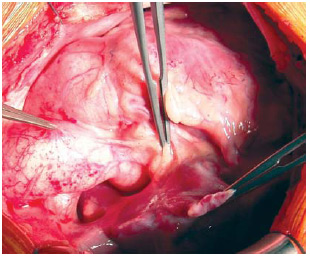
Median transsternal thoracotomy, opening of the pericardium, diagnostic confirmation (Figure 2). Installation of conventional cardiopulmonary bypass (CPB) circuit, using cannulas in the aorta and vena cavae. Induced moderate hypothermia at 28ºC, aortic clamping, opening of the right atrium and interatrial septum and aspiration of the left atrium were all performed. Anterograde, intermittent and hypothermic (4Ú) blood cardioplegia was performed first in the ascending aorta and then after total section of the aorta (directly in the coronary ostia, at 20-minute intervals).
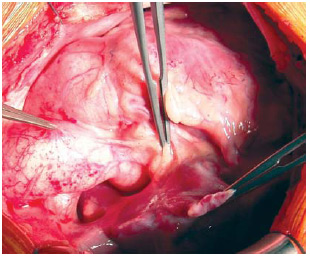
Fig. 2 - External view of the location of the narrowing of the ascending aorta
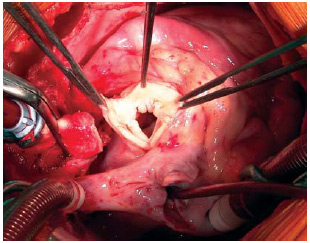
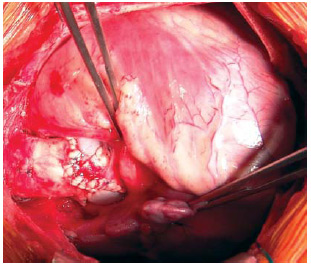
With the aorta transversally sectioned, it is possible to observe the supravalvular ring (Figure 3), which was resected at the beginning of the procedure. Then, three incisions were performed longitudinally towards the sinus, allowing for the implantation of three bovine pericardium patches that were previously cut in diamond shapes and sutured with 5-0 polypropylene threads [3-5]. The ascending aorta was repaired, the air of the cavities was removed and the cavities were sutured; thus, CPB was stopped (Figure 4). The infusion time was 107 minutes and myocardial ischemia was for 66 minutes.
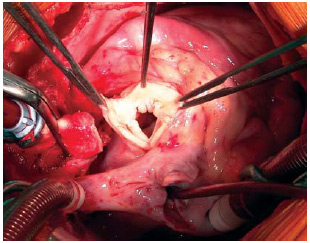
Fig. 3 - Internal view of the aorta after transversal section, showing the fibrous ring to be resected before the longitudinal opening toward the three sinuses
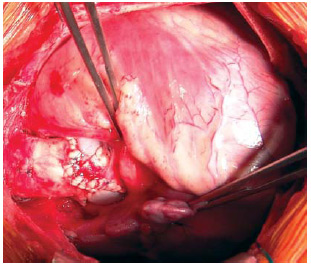
Fig. 4 - Enlarged ascending aorta, repaired using bovine pericardium patches
During the patient's 3-day stay in the ICU, special attention was paid to the pressure control because, with the manipulation of the aorta and the correction of the obstruction, the patient developed severe systemic arterial hypertension. The patient was discharged from hospital on the 14th day after difficulties in pressure control, in excellent clinical conditions, and with the use of furosemide, spironolactone, propranolol and captopril. The echocardiogram showed no stenosis in the ascending aorta, mild aortic valve insufficiency, and pericardial thickening.
After three months, the child is asymptomatic, without medication and with echocardiography showing expanded ascending aorta (without gradient), good ventricular performance and without aortic valve regurgitation.
REFERENCES
1. Kececioglu D, Kotthoff S, Vogt J. Williamns-Beuren syndrome: a 30-year follow-up of natural and postoperative course. Eur Heart J. 1993;14(11):1458-64. [
MedLine]
2. Sylos C, Pereira AC, Azeka E, Miura N, Mesquita SM, Ebaid M. Hipertensão arterial em criança portadora de síndrome de Williams-Beuren (Deleção cromossômica 7q11.23). Arq Bras Cardiol. 2002;79(2):173-6.
3. Stamm C, Friehs I, Ho SY, Moran AM, Jonas RA, del Nido PJ. Congenital supravalvar aortic stenosis: a simple lesion? Eur J Cardiothorac Surg. 2001;19(2):195-202. [
MedLine]
4. Hazekamp MG, Kappetein AP, Schoof PH, Ottenkamp J, Witsenburg M, Huysmans HA, et al. Brom's three-patch technique for repair of supravalvular aortic stenosis. J Thorac Cardiovasc Surg. 1999;118(2):252-8. [
MedLine]
5. van Son JA, Danielson GK, Puga FJ, Schaff HV, Rastogi A, Edwards WD, et al. Supravalvular aortic stenosis. Long-term results of surgical treatment. J Thorac Cardiovasc Surg. 1994;107(1):103-14.
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license