INTRODUCTION
Thymoma is a rare disease even though it is reported as the most common tumor of the anterior mediastinum, involving approximately 20 to 30% of mediastinal masses in adults [1]. It occurs principally in individuals between 50 and 70 years old. Two types have been described, non-invasive, that is encapsulated (around 2/3 of all cases) and invasive.
In relation to its location, 75% occupy the anterior mediastinum, 15% the anterior and superior mediastinum, 6% the superior mediastinum and 4% in other locations [2]. Recently, a case of thymoma of the middle mediastinum was published, which the authors said was the first example in the literature [3]. Subsequently, a second case was reported, in which the patient was successfully treated by surgery, without the necessity of adjuvant radiotherapy [4]. Revision of publications made by Minniti et al. [5] did not find reports of thymomas in the middle mediastinum; these authors described a case of thymoma and one of a thymic cyst in the same region. Venuta et al. [6] emphasized the value of thymectomy in the treatment of myasthenia gravis, as thymomas in 28.4% of the cases negatively influence the prognosis of treatment.
CASE REPORT
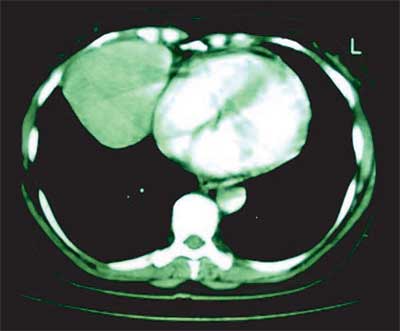
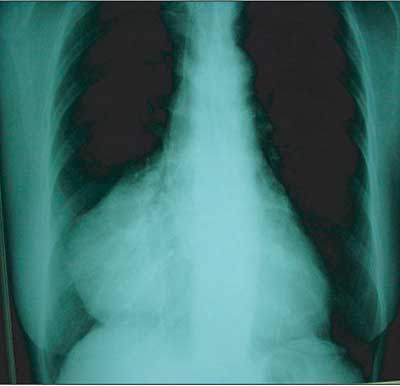
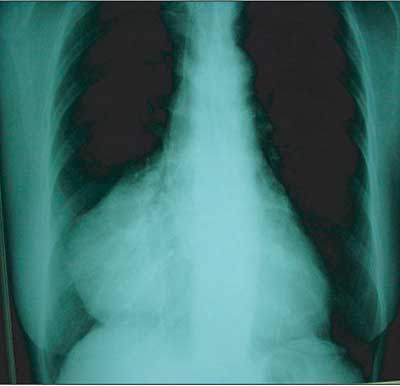
We report on the case of a 55-year-old female Caucasian patient with a history of dysphagia, ptosis palpebral on the left and muscle weakness of the upper limb over a period of approximately 3 months. During the physical examination, she presented with a motor or sensorial deficit, with her motor force preserved at level 3, Glasgow score 15, plantar cutaneous reflex in bilateral flexion and isochoric and photoreactive pupils. She also had problems to close the left eyelid. Using neostigmine there was an improvement in the dysphagia and palpebral ptosis. The patient had not previously used pyridostigmine bromide (mestinon). Biochemical examinations were normal. An image of a mass occupying the middle mediastinum with projection to the right was observed on the chest radiograph. A chest computed tomography revealed presence of a mass in the middle mediastinum, highlighting the necessity of surgery.
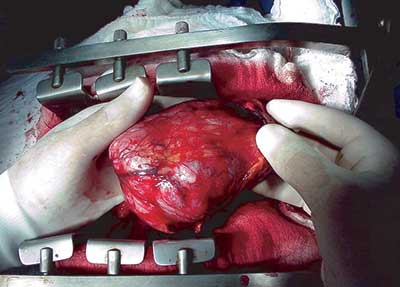
The patient was submitted to median thoracotomy to remove a large mass occupying the middle mediastinum in position beside the pericardium from just under of junction of the superior vena cava with the right atrium, extending laterally to the right and distally in the direction of the diaphragm (Figure 1). An interesting fact was the rare location in the middle mediastinum.
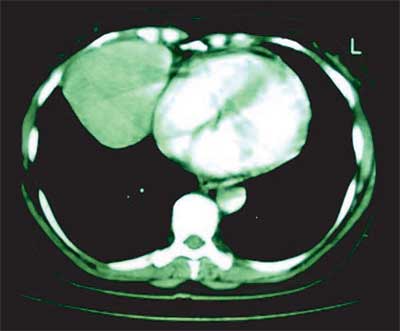
There was no adherence to the mediastinal structures or pericardial and pleural implants. The post-operative evolution was satisfactory and the patient was released from hospital on the 5th post-operative day. A pre-operative computed tomography and chest radiography demonstrated the tumor location (Figure 2). An anatomopathological examination of the sample using optical microscopy and immunohistochemical tests confirmed the diagnosis of thymoma.
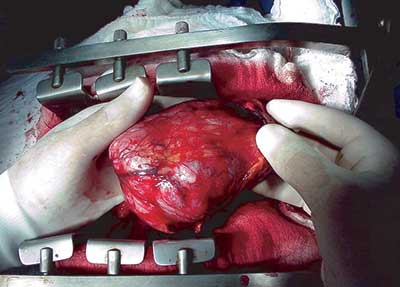
Fig. 1 - Thymoma after separation from surrounding structures occupying the middle mediastinum
A
B
Fig. 2 - Pre-operative computer tomography (A) and chest radiography (B)
Thymomas are slow-growing tumors that generally are benign. Radiographically, thymomas are normally round or oval structures, with well-defined margins that can have some peripheral calcification. Approximately 50% of patients with thymomas suffer from myasthenia gravis and approximately 15% of patients with myasthenia gravis have thymic tumors [7].
Once identified, the treatment of choice is complete resection of the thymoma. In Brazil, patients with benign tumors present 10-year survival rates of 82.6% and with malignant tumors the mean 5-year survival rate is 33.5% [8].
The reported case called our attention because of its location in the middle mediastinum, as normally this tumor is found in the superior and anterior mediastinum. In spite of the size of the tumor with remaining tissue of the thymus located in the anterior and upper regions, the majority of the tumoral was found in the middle mediastinum, which is rare as this is one of the few cases reported in the literature. The report of Kojima et al. [3] describes an extrapleural mass located between the superior vena cava and the trachea, extending up to the azygous vein, under the right innominate artery. This anatomic situation, in our view, does not correspond to the middle mediastinum but in reality, to the upper mediastinum [9]. Kanzaki et al. [4] reported a case of a 60-year-old patient, which is probably the first reported case of a thymoma located in the middle mediastinum. In the same year, Minniti et al. [5] described two other cases of neoplastic masses in the middle mediastinum, only one of which was a thymoma and the other was a thymic cyst. The great experience of Venuta et al. [6] correlated the results of thymectomy in the treatment of myasthenia gravis, concluding that patients suffering from thymomas present an unfavorable prognostic. Everything seems to indicate, from the 232 thymectomies performed by these authors 62 thymomas were located in the upper anterior mediastinum, if not this rare fact would have been mentioned. The case presented by us identified a thymoma located in the middle mediastinum beside the pericardium which is extremely rare. The patient presented signs and symptoms of myasthenia gravis giving a positive response to the therapeutic treatment. By median sternotomy a tumor of 11.50 cm x 7.00 cm x 4.00 cm was removed from beside the pericardium, but without signs of invasion to the pericardium itself. During the same operation the remaining tissue of the thymus was removed with the objective of curing the myasthenia gravis. The results of the anatomopathological examination by optical microscopy were suggestive of thymoma which was confirmed by an immunohistochemical study. The patient was referred to an oncologist for coadjuvant chemotherapy and radiotherapy. Twenty-eight months after the procedure, the patient is in a good clinical state and asymptomatic.
REFERÊNCIAS BIBLIOGRÁFICAS
1. Li JM, Zhou XM, Hu JG. Surgical treatment of 219 cases of primary tumor and cyst of the mediastinum. Hunan Yi ke Da Xue Xue Bao. 2001;26(2):149-51.
2. Ashour M. Prevalence of ectopic thymic tissue in myasthenia gravis and its clinical significance. J Thorac Cardiovasc Surg. 1995;109(4):632-5.
3. Kojima K, Yokoi K, Matsuguma H, Kondo T, Kamiyama Y, Mori K et al. Middle mediastinal thymoma. J Thorac Cardiovasc Surg. 2002;124(3):639-40.
4. Kanzaki M, Oyama K, Ikeda T, Yoshida T, Murasugi M, Onuki T. Noninvasive thymoma in the middle mediastinum. Ann Thorac Surg. 2004;77(6):2209-10.
5. Minniti S, Valentini M, Pinali L, Malago R, Lestani M, Procacci C. Thymic masses of the middle mediastinum: report of 2 cases and review of the literature. J Thorac Imaging. 2004;19(3):192-5.
6. Venuta F, Rendina EA, De Giacomo T, Della Rocca G, Antonini G, Ciccone AM et al. Thymectomy for myasthenia gravis: a 27-year experience. Eur J Cardiothorac Surg. 1999;15(5):621-5.
7. Fraser RG, Pare JAP, Pare PD, Fraser RS, Genereux GP. Diagnosis of diseases of the chest. 3rd ed. Philadelphia:WB Saunders;1991. p.2820-31.
8. Pêgo-Fernandes PM, Ebaid GX, Galizia MS, Marchiori P, Suso FV, Jatene FB. Timoma: discussão sobre tratamento e prognóstico. J Pneumol 2001;27(6):288-94.
9. Di Dio LJA. Tratado de anatomia aplicada. 1a ed. São Paulo:Pólus Editorial;1999.p.308.
 All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license
All scientific articles published at www.bjcvs.org are licensed under a Creative Commons license